Synopsis: This article exposes how women experiencing sleep disruption, pre-menstrual cramping, weight gain, fatigue, and irritability get prescribed antidepressants for what’s actually progesterone deficiency masked as estrogen dominance—not excess estrogen but insufficient progesterone to balance existing estrogen levels. It reveals critical diagnostic gaps including mistimed testing, ignored SHBG levels, and uncalculated progesterone-to-estradiol ratios, while explaining cortisol steal where chronic stress diverts pregnenolone and progesterone toward cortisol production, requiring both stress management and extended-release compounded progesterone for comprehensive treatment.
Top 5 Questions Answered:
- What is estrogen dominance and why is it about progesterone deficiency, not excess estrogen?
- Why do standard hormone tests miss progesterone problems through timing and interpretation errors?
- What is cortisol steal and how does chronic stress deplete progesterone?
- Why does extended-release compounded progesterone work differently than commercial products?
- Why do women who’ve had hysterectomies still need progesterone for breast and brain protection?
Over two decades in compounding pharmacy, I’ve watched the same pattern repeat: Women walk through the door frustrated, holding prescriptions for antidepressants they don’t want to take.
Their doctors heard their complaints—trouble sleeping, pre-menstrual cramping, stubborn weight around the midsection, crushing fatigue, irritability that feels out of control. The response? Start an antidepressant.
But these women aren’t depressed. They’re progesterone deficient.
And the distinction matters more than most people realize.
The Symptoms No One Connects
When a woman describes her experience—can’t fall asleep, can’t stay asleep, extreme cramping the week before her period, weight that won’t budge no matter what she tries, feeling exhausted and irritable—she’s describing a hormonal pattern.
Not a mental health crisis.
Progesterone influences sleep architecture, fluid balance, metabolic function, and mood regulation. When levels drop, all of these systems start to misfire.
The problem is that most women (and many doctors) don’t connect these seemingly unrelated symptoms to one hormone.
Understanding Estrogen Dominance
Here’s what’s actually happening physiologically:
During your menstrual cycle, if ovulation isn’t strong—because you’re not producing adequate estradiol—it affects how much progesterone gets released in the second half of your cycle, the luteal phase.
Estrogen dominance isn’t about having too much estrogen.
It’s about not having enough progesterone to balance the estrogen you do have.
The amount of progesterone your body releases depends entirely on the strength of that month’s ovulation. This can happen at any age, but I see it predominantly in women in their mid-30s and early 40s.
Since 2020, I’ve noticed something alarming: younger women are showing up with these same patterns more frequently than ever before.
What Changed Since 2020
Multiple factors are contributing to earlier progesterone deficiency:
- Environmental toxin exposure
- Lack of exercise
- Increased intake of processed foods
Your body’s hormone production reflects how you live and what you’re exposed to. When those inputs shift, your hormonal output shifts too.
The Diagnostic Gap
When you go to your conventional doctor with these symptoms, testing might happen. But even when it does, it’s often mistimed or misinterpreted.
Here’s what gets missed:
Timing matters. Progesterone should be tested between days 19 and 21 of your cycle—seven days after ovulation, when levels peak. But not all women have 28-day cycles, so this needs to be personalized based on your predicted ovulation date.
SHBG gets ignored. Sex hormone-binding globulin affects how much of your hormones are actually available to use. Most standard workups skip it entirely.
The ratio gets overlooked. Your progesterone-to-estradiol ratio should be at least 50 to 1. Most doctors don’t calculate this because it requires converting between picograms and nanograms—a step that gets skipped.
When your ratio comes back at 30 to 1 instead of 50 to 1, you feel it in every aspect of your life.
What That Ratio Feels Like
Some women are more sensitive than others, but when estrogen dominance persists over time, the consequences compound:
- Gallstones
- Fibroids
- Diverticulitis
- Heavy menstrual bleeding and severe cramping
- Intense anger and irritability the week before menstruation
You wake up tired. You go to bed wired.
Your body feels like it will never get enough sleep to recover.
The Cortisol Connection
That “tired but wired” feeling often signals another layer to the problem: cortisol steal.
All steroid hormones start with cholesterol converting to pregnenolone. Pregnenolone then serves as the shared precursor for progesterone, DHEA, and cortisol.
Under chronic stress, your body prioritizes survival.
The hypothalamic-pituitary-adrenal axis activates, increasing cortisol-producing enzymes and pulling pregnenolone and progesterone down the cortisol pathway to meet immediate demands.
Progesterone declines first because it’s both a functional hormone and a cortisol precursor. Less remains available for menstrual balance, neurocalming effects, and estrogen regulation.
DHEA production gets suppressed as well, creating a low DHEA-to-cortisol ratio.
The result? Cortisol dominance with reduced progesterone and DHEA, contributing to sleep disruption, anxiety, blood sugar instability, fatigue, and impaired hormone balance—even when your cortisol levels look “normal” on standard testing.
Treatment That Addresses Both
You can’t just replace progesterone without addressing the stress piece.
When I work with patients who have both cortisol steal and progesterone deficiency, we start with stress management:
- Meditation
- Yoga
- Journaling
- Making a list to prioritize and minimize controllable stressors
If lifestyle modifications aren’t enough, adaptagenic herbs help manage cortisol levels. I often recommend ashwagandha, rhodiola, or holy basil.
But here’s where personalization matters: Some adaptagens increase testosterone, others help lower it. For a woman with PCOS, that distinction is critical.
I evaluate testosterone levels before recommending any adaptagenic herb.
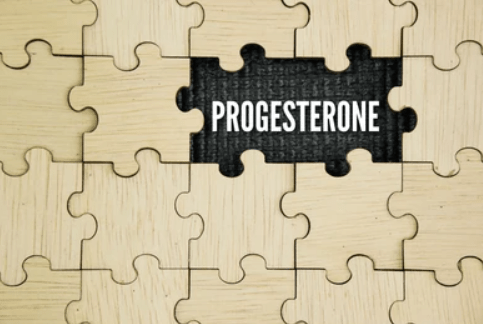
Why Compounded Progesterone Works Differently
The compounded version I recommend contains E4M, an inert ingredient that allows progesterone to be absorbed over an extended period.
Progesterone works quickly in your body. Commercially available products get immediately absorbed and used. For women struggling with sleep—both falling asleep and staying asleep—that immediate absorption helps with falling asleep not staying asleep.
The extended-release formulation matches how your body actually needs progesterone throughout the night.
Dosing That Matches Your Biology
The right dose depends on your hormone levels combined with your specific symptoms.
I recommend anywhere from 25 mg to 200 mg. At a compounding pharmacy, they can customize to any dose in between.
That range shows why one-size-fits-all approaches fail. Your biology, your symptoms, your stress levels, your age, your cycle—all of these inform the right dose for you.
What You Need to Know
Progesterone is extremely safe.
The name itself—pro-gestational—reflects that we produce it during pregnancy. It’s not associated with increased cancer risk.
Even if you’ve had a hysterectomy, you need progesterone. Your breasts need protection. Your brain needs protection.
Women who’ve had hysterectomies are often told they don’t need progesterone anymore. That advice ignores how this hormone functions beyond the uterus.
The Shift I’m Seeing
Women are intuitive. When they visit their doctor seeking better health and get told their labs are normal, they know something’s off.
They know an antidepressant isn’t the right answer.
What gives me hope is watching more women trust that intuition. They’re asking better questions. They’re seeking providers who look for root causes instead of prescribing symptom management.
This article exists to give you hope that there is a root cause answer—using a bioidentical hormone, not a drug that’s foreign to your body.
Your symptoms are real. Your experience is valid.
And there’s a better path forward than the one you’ve been offered.