The standard advice for menopausal bone health is the biggest load of nonsense I’ve ever heard.
“Just take some calcium, sweetie, and maybe a little Vitamin D.”
The whole system treats osteoporosis like your bones just ran out of chalk. Like we can dump some calcium supplements into your body and everything will magically rebuild itself.
Here’s what actually happens: about 20% of bone loss occurs in your first five years of menopause. During that critical window, your skeletal system is undergoing a dramatic transformation that most women aren’t warned about until it’s too late.
And calcium alone? It’s like dumping construction materials on a sidewalk without a foreman to direct where they go.
The Foreman Your Bones Are Missing
Your body doesn’t have a calcium deficiency problem. It has an instruction problem.
Think of bone health like a construction site. You need materials, yes. But more critically, you need a high-level management team giving precise instructions about what to build, where to build it, and when to stop tearing down the old structure.
That management team is your endocrine system. And when menopause hits, the Head Architect walks off the job.
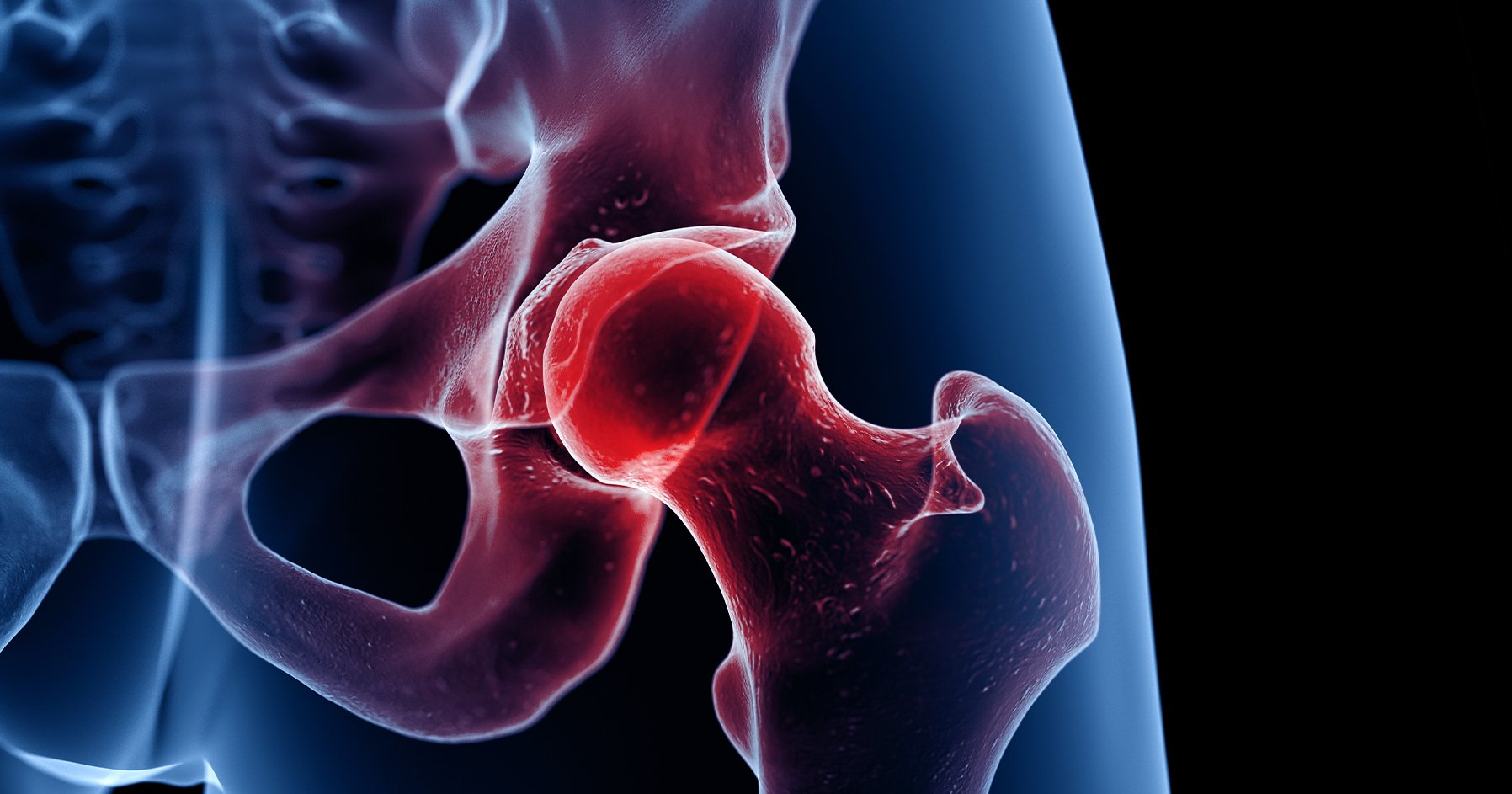
Estradiol is that Head Architect. Her main instruction is simple but critical: stop the wrecking crew from breaking down old bone faster than it can be rebuilt.
When estradiol drops during menopause, the wrecking crew (osteoclasts) goes wild. Your bone density plunges.
But estradiol isn’t working alone. You’ve got Testosterone and DHEA acting as Structural Engineers, stimulating the builders (osteoblasts) to create new, dense bone. You’ve got Parathyroid Hormone as the Regulator, constantly monitoring calcium levels and pulling from the bone bank when blood calcium dips. And you’ve got Thyroid Hormones as the General Contractor, regulating the overall metabolic rhythm of bone turnover.
The conventional calcium-only approach ignores this entire chain of command.
Without the right hormonal instructions, all that calcium is just floating around. Maybe it settles in your arteries instead of your bones. Maybe it does nothing at all.
We’re treating a construction project like a supply problem when it’s actually a management crisis.
Catching the Wrecking Crew in Action
I don’t guess about bone health. I measure it.
When estradiol pulls her protective signal, the wrecking crew gets loud. And we can catch them in the act through a urinary biomarker called N-Telopeptide Crosslinks (NTX).
NTX measures fragments of bone’s collagen protein released into urine when old bone breaks down. Think of it as measuring construction debris.
When NTX levels are high, it confirms the osteoclasts are aggressive, resorbing bone much faster than the builders can keep up. The woman is in a state of net bone loss.
High levels of bone resorption markers are associated with approximately 2-fold increased risk of osteoporotic fractures.
I also look at the hormones that should be controlling that action. If estradiol is below optimal functional levels, the Head Architect is missing. If Parathyroid Hormone is elevated (often due to low Vitamin D), the Regulator is panicking, constantly raiding the bone bank.
A combination of high NTX coupled with low estradiol and low Vitamin D is definitive proof the wrecking crew is running wild.
It’s time to intervene aggressively. We’re not guessing. We’re using the debris count.
The Personalized Hormone Strategy
When I see those high NTX levels screaming “accelerated bone loss” alongside low estradiol, I never reach for a pre-printed prescription pad.
We aren’t treating a number. We’re treating a powerful, complicated woman with a unique history.
Before we talk dosing, we talk life. I conduct a thorough history review covering everything from current symptoms (sleep, mood, pain) to family history (stroke, breast cancer, osteoporosis). We look at her exact stage in life, whether she’s in perimenopause or post-menopause.
This foundational narrative is non-negotiable.
Hormones don’t work in a vacuum. We assess lab results, lifestyle stressors, and dietary intake. This gives crucial context for the minimum therapeutic dose she’ll need.
For bone health, the goal isn’t to shock the system. It’s to provide consistent, gentle instruction needed to quiet the wrecking crew.
We start with a low dose of bioidentical estradiol and titrate slowly. Then we check back in within a few months, review symptoms, and most importantly, re-test those NTX levels.
The change in her NTX is objective proof that estradiol is effectively delivering the instructions needed to slow bone loss.
We titrate the dose until we hit the sweet spot where her symptoms are resolved and her NTX markers show marked improvement.
This isn’t guessing. It’s precise, proactive, and personalized to preserve her long-term structural health.
Why Oral Estradiol Wins for Bones
Delivery method matters more than most people realize.
Both oral and transdermal estradiol preserve bone density. But the strongest evidence for reducing actual fracture risk comes from large-scale trials of oral estrogen.
The Women’s Health Initiative found a 33% reduction in fracture risk with hormone therapy. That’s not just better numbers on a DEXA scan. That’s fewer broken hips, fewer vertebral fractures, fewer life-altering injuries.
Oral estradiol has another advantage: the first-pass effect through the liver.
This metabolic pathway improves cholesterol profiles by favorably affecting the ratio of HDL to LDL. For a woman whose greatest long-term risk is cardiovascular disease, this effect provides powerful, quantifiable protection that transdermal routes can’t replicate.
You’re getting maximum cardiovascular protection alongside bone benefits.
For the healthy woman without clotting risk factors, oral estradiol is often the superior choice for maximizing long-term protection of bone, heart, and brain.
The Exercise Most Women Skip
Walking won’t save your bones.
I know that’s not what you want to hear. Walking is great for cardiovascular health. But it doesn’t provide enough impact shock to signal bone growth, especially in the hips and spine where most osteoporotic fractures occur.
Your bones respond to force. Specifically, they respond to compression forces that travel directly through the skeletal system.
I prescribe what I call the three pillars of physical fitness for longevity: strength, balance, and flexibility. These give a woman the tools to protect her bones from fracture.
The Weighted Goblet Squat encompasses all three.
Hold a heavy dumbbell or kettlebell against your chest. This forces activation of the core, glutes, and quadriceps. Perform the squatting movement slowly and controlled, which requires intrinsic stability and balance throughout the kinetic chain. Achieve depth in the squat to improve hip and ankle mobility.
When you descend into a Weighted Goblet Squat and forcefully drive up, the load is significantly higher than body weight. This creates a powerful force that travels directly up the kinetic chain, compressing the femur and lumbar spine.
This high-level force is the strongest signal your body has to activate osteoblasts and improve bone mineral density.
I recommend weighted, multi-joint movements that apply maximal, controlled strain to the exact sites most vulnerable to fracture.
It’s not about being “active.” It’s about being strong and stable under load.
The Nutrient Trio That Actually Works
Bone is approximately 50% protein by volume, mostly collagen.
Without adequate protein, the best minerals in the world have no scaffolding to stick to.
The synergistic bone-building combination I’ve seen make measurable differences is: Protein (Collagen Peptides) + Vitamin K2 + Vitamin D3.
I recommend 15 to 20 grams daily of high-quality collagen peptides for joint and bone matrix synthesis. This ensures the body receives a significant bolus of necessary amino acids to drive collagen production, especially in older adults who may have diminished endogenous collagen synthesis.
Research on specific collagen peptides found that postmenopausal women taking them daily showed 4.2% higher BMD in the spine and 7.7% higher BMD in the femoral neck compared to placebo after just 12 months.
Timing matters. Take collagen immediately following strength training because combining the mechanical stimulus of exercise with rapid amino acid availability maximizes the repair and growth signal for both muscle and surrounding bone.
But protein alone isn’t enough. Calcium and magnesium need two key vitamins to ensure they’re properly utilized by bone rather than floating in the bloodstream or depositing in soft tissues.
Vitamin D3 regulates calcium absorption in the gut. Without sufficient Vitamin D3, only a fraction of dietary calcium gets absorbed. A healthy serum level of 50-80 ng/mL is directly correlated with lower NTX levels and better BMD.
Vitamin K2 (as MK-7) is the traffic cop for calcium. It activates osteocalcin (which binds calcium to the collagen matrix in bone) and Matrix Gla Protein (which inhibits calcium deposition in arterial walls).
By activating these proteins, K2 ensures that calcium absorbed by D3 is specifically directed to bone while staying away from arteries.
This is how you build bone while protecting cardiovascular health simultaneously.
Beth’s Transformation
Beth came to my practice almost two years ago. She was 62, postmenopausal for a decade, and her trajectory was rapidly moving toward severe osteoporosis.
She presented with hot flashes, joint pain, insomnia, vaginal dryness, low libido, and significant anxiety. Her initial labs showed suboptimal Vitamin D at 28 ng/mL. Her DEXA scan reported osteopenia bordering on osteoporosis.
Her first NTX was elevated in the mid-40s, indicating a high rate of bone breakdown.
The hardest part wasn’t designing her protocol. It was getting her to stick with it.
Beth was initially terrified of estradiol. She’d gone 10 years without hormone therapy and worried about theoretical risks like blood clots and cancer. This led to missed doses at the beginning.
She also viewed lifting heavy weights as a risk for joint injury. She defaulted to light cardio and low-impact movements that wouldn’t provide the necessary mechanical loading signal for bone growth.
What finally shifted her perspective was that elevated NTX lab result.
A concrete, measurable number showing her bone was dissolving faster than it was rebuilding. This transformed vague fear into actionable risk.
I explained the benefits of the treatment plan and the importance of compliance. After several months of hard work and improved lab results, Beth realized oral estradiol wasn’t a risk to be feared. It was perhaps the most powerful antidote to the actual immediate risk of high bone turnover.
Once she pushed through initial discomfort and started seeing rapid improvement in physical strength and joint pain (due to anti-inflammatory effects of hormones and exercise), weight training became intrinsically rewarding.
She realized the weights weren’t breaking her. They were literally making her anti-fragile.
This positive feedback loop locked in her adherence to both exercise and the hormone regimen.
Over 18 months, we implemented oral bioidentical estradiol and progesterone, high-dose Vitamin D supplementation, daily collagen peptides with a Vitamin C source for improved absorption, and a structured physical activity routine focusing on strength training, yoga for balance, and flexibility work.
Her repeat DEXA scan showed bone density improvement. Her NTX lab marker decreased to an optimal level.
The combination of oral estradiol (for the systemic signal), targeted nutrients (for the raw material), and high-impact strength training (for the mechanical signal) reversed years of bone loss.
Beth’s case is a powerful reminder that bone health is highly responsive when you address the entire system.
Why Doctors Keep Getting This Wrong
The default to “just take calcium” advice stems from systemic, educational, and logistical factors within conventional medicine.
Our traditional healthcare system compartmentalizes the body into siloed specialties. Bone health gets treated as a single-system disease managed by specialists or primary care physicians following highly specific, linear protocols.
The connections functional medicine uses (hormones, gut health, strength training) often fall outside the scope defined by those cookie-cutter protocols.
There’s also an evidence hierarchy that heavily favors large, randomized controlled trials. Much of the comprehensive evidence (nutrients, exercise types, personalized dosing) comes from smaller, mechanistic, or observational studies considered “softer” evidence than massive pharmaceutical trials.
Medical school and continuing education are heavily influenced by data on FDA-approved drugs. The immediate, measurable efficacy of a drug like a bisphosphonate in halting bone loss is seen as more reliable and legally defensible than a long-term, multi-modal lifestyle plan.
Then there are logistical barriers built into the structure of traditional healthcare visits.
A typical primary care appointment is 7 to 15 minutes. It’s physically impossible to conduct a thorough risk-benefit analysis encompassing a patient’s cardiovascular risk, brain function, exercise routine, personalized nutrient status, and historical facts in that window.
Prescribing a simple calcium supplement is fast and easily documented.
Conventional doctors aren’t typically trained or reimbursed for being expert dietitians or personal trainers. They lack the resources to design and oversee a progressive functional treatment plan.
The fear of liability is real. Physicians often default to standard-of-care guidelines to minimize legal risk. The standard of care for osteoporosis is to try generic calcium and Vitamin D, then move directly to a bisphosphonate.
Diverging into a sophisticated hormone and nutrient plan is seen as a deviation from the established, liability-minimizing path.
While doctors genuinely want to help, the system they operate within forces them to prioritize speed, adherence to standardized protocols, and pharmaceutical solutions over time-intensive, root-cause resolution.
What Medical Schools Should Teach Instead
If I could change one thing about how medical schools teach future doctors about menopausal bone health, it would be this: shift from a Disease Management Model to a Prevention and Healing Model focused on Hormone and Structural Physiology.
Instead of framing osteoporosis primarily as a calcium-deficiency disease to be treated with pharmaceuticals, medical schools should teach that bone is an endocrine-responsive, load-bearing organ.
Its health is maintained by a delicate balance of hormones, nutrients, and mechanical force.
Future doctors must understand that the post-menopausal drop in estradiol is the root cause of accelerated bone loss. This validates the use of hormone therapy as a foundational, first-line treatment for the vast majority of symptomatic women, rather than reserving it as a last resort.
This practical, patient-centered model would equip new doctors with critical thinking skills to address root causes and recommend comprehensive, synergistic therapies.
Moving beyond the simple calcium band-aid to true physiological restoration.
Because one out of three women over 50 will experience an osteoporosis-related bone fracture. Most will suffer decreased mobility, function, and quality of life.
We can’t afford to keep dumping materials on the sidewalk and hoping for the best.
We need to bring back the foreman. We need to give women the hormonal instructions, the nutritional scaffolding, and the mechanical signals their bones are desperately waiting for.
That’s not radical medicine. That’s just good construction management.
Donna Figueroa, CNM, FMACP, MSN, APRN
Donna is passionate about guiding women through midlife transformation. She is a Certified Functional Medicine Provider, Licensed Nurse Practitioner, and Board-Certified Nurse Midwife who has spent the last 15 years caring for women across the lifespan and solving medical mysteries for many who have otherwise been unable to find resolution elsewhere.
In 2015 Donna found herself in the throes of perimenopause, 40 pounds overweight with excruciating joint pain, 2 failing hips, a dependence on NSAIDs, thinning hair, weak nails, and hot flashes galore. Her physical therapist told her she needed double hip replacement surgery. Instead of going under the knife and falling prey to worsening menopausal symptoms, Donna researched alternatives and discovered the wonders of Functional Medicine!
Within weeks, her pain resolved; Donna avoided surgery, discontinued taking NSAIDs, and lost 40 pounds by addressing the root cause of her chronic inflammation, changing her lifestyle, altering her diet, and reducing toxic exposures.
Donna even turned back her biological clock, which currently registers at 14 years younger than her chronological age.
Donna’s health transformation fueled her enthusiasm and desire to help others achieve the same success, and she is committed to providing guidance and support to anyone who is determined to do… Read more