Bladder leakage is often referred to as urinary incontinence. It is simply the involuntary/ accidental discharge of urine. In the United States, studies from the National Association for Continence have shown that more than 20 million adults experience urinary incontinence of varying severity.
In more elaborate terms, over 25 million Americans experience different forms of incontinence, ranging from temporary to severe/chronic incontinence. In most cases, urinary incontinence is caused by aging. However, incontinence is not a factor in aging. While most cases of incontinence are caused by aging, many people still go on to live many years without experiencing any form of incontinence.
Urinary Incontinence in Women

Bladder leakage in women can occur at any age. However, it is more common in menopausal women or women over 50. In the United States, more women suffer from incontinence than men. Women are more affected because as they progress through different life phases, like pregnancy, childbirth, and menopause, they become more exposed to problems related to bladder control.
Causes of Urinary Incontinence
Bladder control is very important, especially for humans. There’s always a space for bathrooms in homes, offices, parks, gyms, concerts, and even on beaches and pools. The ability to hold urine even when we shouldn’t have always been so important. However, certain conditions can jeopardize this widely appreciated ability.
In both men and women, incontinence is mostly caused by dysfunctions or the inability of the muscles and nerves supporting the bladder to operate optimally. However, underlying conditions and illnesses usually cause the decreased functionality of these vital muscles and nerves. Many of these conditions are distinct to the female gender, making women more susceptible to incontinence. The bladder would struggle to hold urine with the muscles and nerves weakened.
Constipation, rapid weight gain, and surgery are the common causes of urinary incontinence. However, the most common causes of incontinence in women are pregnancy, childbirth, and menopause.
How Pregnancy Triggers Incontinence
More than 40 percent of women experience varying severity of incontinence during pregnancy. Incontinence during pregnancy is caused by the pressure exerted on the pelvic organs by the fetus. As the unborn baby grows in the uterus, the uterus gets bigger, suppressing vital organs in the pelvic region, like the urethra, the bladder, and the pelvic floor muscles. As the baby stays in the womb for a long time, the pelvic floor muscles become weakened and temporary cases of incontinence are experienced.
In most cases, the pelvic floor muscles will heal over time. However, many women still experience incontinence after 2 months of childbirth. In these cases, the woman is advised to visit the hospital or talk to a qualified medical practitioner.
Effects of Childbirth on Incontinence

In some cases, complications during childbirth can damage the nerves controlling the bladder, weaken the pelvic floor muscles even further and extend incontinence for longer periods. Nevertheless, the pelvic floor muscles are expected to heal with time. If incontinence lasts up to 6 weeks, the woman is advised to visit the hospital or talk to a qualified medical practitioner.
Urinary incontinence caused by pregnancy and childbirth is temporary and will only last for a few weeks. However, incontinence caused by menopause can last longer, even for many years.
How Menopause Triggers Incontinence
Owing to the ability of the ovaries to produce important hormones like estrogen, progesterone, and testosterone, menopausal women, are bound to experience hormone fluctuations caused by the decline in the ovaries’ functionality. The fluctuation in hormonal levels is the main cause of many symptoms experienced by menopausal women today. Some symptoms include hot flashes, night sweats, osteoporosis, urinary incontinence, bloating, weight gain, cardiovascular diseases, and certain cancers.
Studies have shown that the drop in hormonal levels can weaken the urethra, leading to incontinence. The urethra is important for regulating urine in the bladder which means that any slight tampering in the urethra can affect bladder control.
Furthermore, the average start time for menopause is 52 years. At 53, the youthful feel of the body tends to go away, and with time, many body organs are weakened.
Organs like the pelvic floor muscles and the urethra can be affected by age, which is why incontinence is more common in older adults. With hormonal fluctuations in the bladder during menopause clashing with the effects of aging on the same organs, menopausal women at 60 and beyond are twice more likely to develop incontinence than men and the same age.
In most cases, older adults do not just pee on themselves. What happens is that the bladder becomes unable to hold as much urine as it did in previous years. It means that frequent visits to the bathroom can be imminent.
Types of Urinary Incontinence
Urinary incontinence comes in different forms. Some types of incontinence include:
Stress Incontinence
This type of incontinence happens when the bladder is subjected to external pressure like exercises, sneezing, laughing, coughing, and other physical conditions. In stress incontinence, the bladder holds urine quite well under serene circumstances.
However, small pressure on the bladder will cause bladder leakage. Sometimes, the pelvic muscles are effective enough but can withstand pressure. Many women experience small leaks from below when they engage in exercises like skipping rope or even coughing and laughing.
Functional Incontinence
In functional incontinence, the bladder is perfectly fine. However, the problem comes from difficulty reaching the restroom on time. Functional incontinence is caused by disabilities that impair movement so badly that it becomes difficult or impossible to reach the restroom. Conditions like disabilities, arthritis, and injury may make an individual urinate at a spot when the bladder is full already without getting to the restroom.
Urgency Incontinence
Urgency incontinence, in most cases, is caused by an underlying condition. Urgent incontinence means the bladder cannot hold urine long enough to reach the restroom. Unlike in functional incontinence, where reaching the restroom is the problem, the problem in urgency incontinence is holding the urine long enough to reach the restroom. Urgency incontinence is the most common form of incontinence in both men and women.
A characteristic feature of urgency incontinence is frequent visitation to the bathroom and the constant urge to urinate.
Overflow Incontinence
When the bladder cannot accommodate more urine, the individual will most likely find it difficult to hold it any longer. When the capacity of the bladder is reached, incontinence becomes almost imminent. Most people have experienced overflow incontinence.
However, doctors and other medical professionals strongly advise against leaving the bladder to reach its peak capacity. It is important to go to the restroom immediately after you feel the urge to urinate.
Symptoms of Urinary Incontinence
Urinary incontinence is not regarded as a disease. Rather, it is a symptom of an underlying illness or condition. Many of these diseases will cause the weakening of the pelvic floor muscles, which will cause incontinence of varying severity. However, people with incontinence often experience other symptoms triggered by problems related to bladder control.
Some symptoms of incontinence include:
- Frequent visits to the bathroom. Medical elites frequently suggest more than twice at night or anything more than 8 times during the day.
- Pain, discomfort, or just some pressure in the pelvic region. In most cases, the pain felt in the pelvic region will cause frequent visits to the bathroom, even when urine is held to some degree.
- Bedwetting.
Diagnosis of Incontinence
A doctor or a nurse carries out a diagnosis of incontinence. During diagnosis, questions regarding the general medical history and the symptoms felt are asked. After asking questions, doctors or nurses usually have a diagnosis already. However, some physical tests must be conducted to diagnose precisely.
Some tests performed in the diagnosis of incontinence include:
Urine Test
A urine test involves taking a sample of one’s urine to the lab for infections or perceived causes of incontinence.
Ultrasound
In ultrasound, the doctor uses an ultrasound wand to take pictures of specific parts of organs in the pelvic regions. These organs include the bladder, the urethra, and the kidneys. The doctor checks for anything odd and anything capable of causing incontinence.
Bladder Stress Test
The bladder stress test is a physical examination performed by the doctor to check for any loss of urine when pressure is exerted on the pelvic region. In this test, the doctor can tell the patient to laugh, cough, or sometimes add physical pressure to the pelvic region to check for loss of urine.
Cystoscopy
In this test, the doctor uses a camera attached to a tube to observe and check for signs of damaged tissues. The tube is inserted into the urethra and the bladder.
Urodynamics
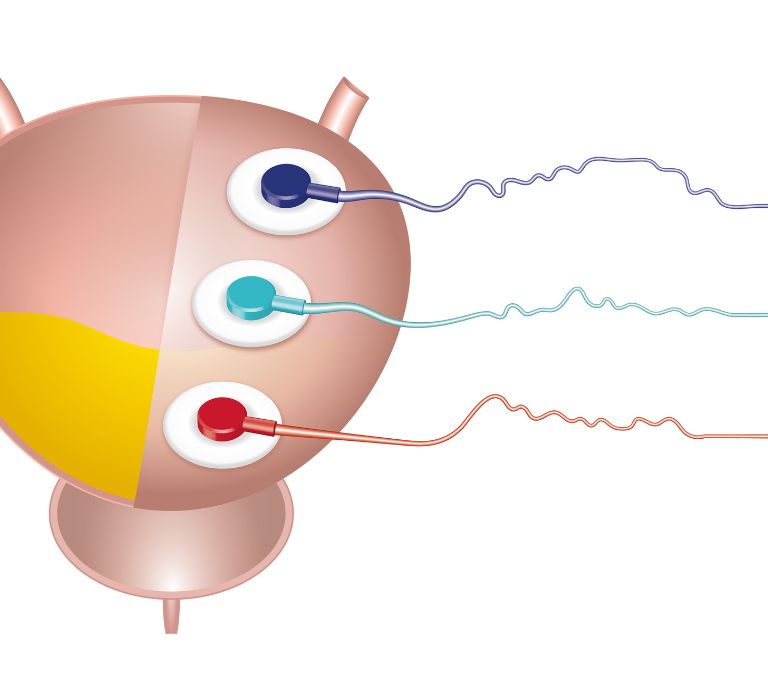
Just like cystoscopy, urodynamics also involves the insertion of a tube into the urethra. The difference between cystoscopy and urodynamics is that no camera is attached to the tube in urodynamics. Instead, the doctor inserts a tube and then fills the bladder with water. After doing this, the doctor carefully measures the quantity of pressure required to cause involuntary bladder leakage.
Treatment of Incontinence
In many cases, the condition causing urinary incontinence is treated in a bid to resolve issues with incontinence. However, incontinence is treated separately in other cases.
The doctors and nurses are responsible for drafting a treatment plan for the problem.
Kegel Exercises
Also known as pelvic floor muscle training, kegel exercises are physical activities to strengthen the pelvic floor muscles to manage or treat incontinence. Since the pelvic floor muscles help support the pelvic region’s organs, strengthening them can help prevent, manage, or treat incontinence. Studies have shown that up to 40 percent of women with incontinence experience improved results from engaging in kegel exercises.
While kegel exercises seem to have no wrongs attached to them, it is important to know that sometimes, kegel exercises may worsen incontinence. Sometimes, bladder leakage is caused by over-tightened pelvic floor muscles, and making the muscles even tighter can increase the severity of incontinence. Overly tightened pelvic floor muscles are overworked and can weaken over time. For this reason, women are advised to see a doctor before engaging in kegel exercises.
How to Do Kegel Exercises
Kegel exercises are done to strengthen the pelvic floor muscles. That space between your vagina and your butthole is where your pelvic floor muscles are. Generally, kegel exercises involve lying down, squeezing the muscles in your genital area, relaxing them, and then squeezing them again until you’re satisfied with the process. However, you may decide to make it more exciting by practicing the following techniques:
Bridge
This exercise strengthens the buttocks but can also help toughen the pelvic floor. To perform the “bridge,” follow the following instructions.
- On the floor, rest on your back and bend your knees. In this position, your feet should be flat on the floor. Ensure your arms are placed at the sides with your palms faced down.
- While in this position, contract your buttocks and pelvic floor muscles. As you tighten, lift your buttocks several inches from the ground.
- Remain in this position for at least 3 seconds and, at most, 8 seconds
- After this, relax the buttocks and muscles of the pelvic floor as you lower your buttocks back to the ground.
- Take a quick rest and perform more sets.
Gentle Jumps
This exercise is similar to squatting. What makes it different is that instead of squatting on the spot, you take gentle jumps before going back down.
The steps are as follows:
- Stand on both feet, having them wide apart and keeping them flat.
- Bend until your buttocks almost come in contact with the floor. Keep on going low until you feel you can’t go any further.
- While doing this, ensure you keep your back straight and, at the same time, tilt it slightly forward. At this point, the knees should be relatively straightforward to the toes.
- As you go back up, jump gently and come back down.
- Repeat this process five times.
Vaginal Lasers
The use of vaginal lasers for treating incontinence in women is still developing. The first use of vaginal lasers for incontinence was performed as early as 2014. Vaginal lasers are non-surgical and non-invasive treatment options that serve as effective treatment options for urinary and sexual symptoms caused in most cases by menopause.
As the name implies, vaginal lasers function predominantly by using lasers. During operation, a laser sends enough energy through a medium to heat the vagina tissues to cause the growth of new collagen.
With the action of these lasers, new collagen can be effectively grown in regions around the urethra, strengthening the tissues and reducing incontinence. While studies on the effectiveness of lasers on incontinence have been quite limited, many women have reported significant improvements in urinary incontinence problems after vaginal lasers administration.
Side Effects of Vaginal Lasers
Side effects involved in the use of vaginal lasers include infection from unsterilized tools, bleeding, bruising, redness, and numbness. In some uncommon cases, vaginal lasers can cause complications like painful intercourse, unprecedented death of tissues, and serious infection that could last for several years. Women are advised to make due consultations with a qualified medical practitioner to get more information on the side effects of vaginal lasers.
Cost of Vaginal Lasers
Since the need to get more non-surgical treatments have increased over the years, the cost of vaginal lasers has also increased. Generally, vaginal lasers cost between $1,300 and $4,600. The cost can change depending on the number of times required to do the procedure or the treatment location.
Access to Vagina Lasers
The use of vaginal lasers is still controversial owing to the risks involved. Despite the approval by FDA, many believe medical practitioners should stop vaginal rejuvenation lasers. However, vagina laser treatment is available in clinics and online. You can book a session with a qualified medical practitioner. However, ensure a comprehensive discussion with a doctor before attempting vagina rejuvenation laser treatment.
Platelet Rich Plasma Therapy (PRP)
This treatment option may help treat women with incontinence. It involves tightening the vaginal tissues and facilitating the growth of natural collagen used by the body. PRP is an all-natural procedure that involves drawing blood from the body and then placing the blood in a centrifuge in a bid to obtain platelet-rich blood.
After spinning in a centrifuge, the platelet-rich blood is injected back into the body, but this time, into the vagina. This way, the vagina tissues are tightened. PRP helps support cell growth and can form clots in the vagina to help heal any form of injury.
PRP is widely used today for helping women achieve orgasms and experience satisfying sex. However, recent techniques have used this treatment for incontinence. By tightening the vagina, PRP can help women achieve better bladder control. PRP has been very effective in promoting effective sexual and physical health in women, from a decline in libido to the inability to control the passage of urine.
Side Effects of PRP
With the low-risk and all-natural procedure of platelet-rich plasma therapy, the side effects are minor and will not result in any health risk of major concern. Side effects aren’t very common, but if they appear, they can come in the form of infection, pain at the injection site, tissue damage, and nerve injuries. While PRP is generally an effective treatment option with low risks, it is important to talk to a doctor before going for one.
Cost of PRP
The cost of PRP ranges from $500 to $2500. Depending on the location, the cost of PRP can vary; sometimes, repeat treatments are required to get an optimal solution to the problem. The cost can also change depending on the expertise of the doctor and the. Some insurance plans in the United States cover PRP treatments.
Availability of PRP Treatment
Many hospitals and clinics in the United States and Canada offer effective PRP treatment. Generally, PRP can be easily accessed in most countries of the world.
Women’s Sexual Health
Sexual health influences general health. Many women see sexual health as just healthy sex. However, sexual health goes beyond just healthy sex. The health and well-being of many women today are often affiliated with sexual health. Sexual health defines every woman’s physical, mental, social, and emotional health. According to the WHO, aspects of sexual health include:
- Reproductive health and fertility
- Knowledge of the risks involved in sex and other sexual activities
- Safe and pleasurable sexual experiences
- Violence-free relationships
- Understanding sexual identities
- Access to good healthcare and top-notch educational resources to achieve optimal sexual health
The reproductive system of women is more elaborate and complex than the reproductive system of men. Unlike in men, the reproductive system is more open. The openness of the female reproductive system is the main reason women suffer more from diseases and infections of the reproductive system than men. Due to the delicacy of the reproductive system, optimal maintenance is paramount.
In men, the desire for sex is often provoked by sexual arousal. In women, this is not always the case. Women often have sex when provoked by sexual arousal. However, many women engage in sexual activities for companionship and the desire to please their partners.
As women age, their libido decreases, reducing their desire for sex. For many women, the idea of sexual health is centered on contraception. For other women, sexual health is centered on disease prevention. Whatever your definition of sexual health, the aim is always to maintain a healthy and balanced reproductive system.
As women go further in age, they experience very significant changes in their reproductive system. From puberty to pregnancy, childbirth, and menopause, the female reproductive system is constantly changing, and how you react to it will make it better or do otherwise. Women are strongly advised to take precautions to avoid problems with the reproductive system.
Practice Safe Sex
The concept of safe sex is quite simple. It refers to taking measures to prevent the exchange of bodily fluids like blood, semen, saliva, and vaginal secretion during sexual activities. Physical barriers like external and internal condoms, gloves, and dental dams prevent exchanging or sharing these fluids. These physical barriers can help prevent diseases like HIV, chlamydia, trichomoniasis, gonorrhea, and hepatitis A, B, and C. While these barriers cannot guarantee 100 percent prevention of STIs, they can reduce your risk of contracting them.
Practicing safe sex can also help with birth control. Since the semen doesn’t enter the vagina when having sex with someone who has sperm, pregnancy is prevented. This option is important for women who aren’t ready to bear children or do not want children for several reasons but still want to enjoy the pleasure of sexual activities.
Vaginal Hygiene
Vaginal health is very important. While the United States has achieved so much regarding the enlightenment of girls and women on the importance of good vaginal hygiene, countries like India are still lagging. An unhealthy vagina introduces a woman to very complicated illnesses that are often severe. Maintaining a healthy vagina is paramount for every woman worldwide, from problems with libido to infertility. Just like girls today learn science and history, vaginal hygiene should be equally important.
Some measures to maintain good vaginal health include:
- Keeping the undergarments dry to prevent infections from damped panties caused by vaginal fluid
- Changing sanitary pads every 6 hours
- Avoiding the use of soap for washing the vagina
- Cleaning the vagina after intercourse
- Practicing safe sex
- Avoiding tight clothes
Since time immemorial, maintaining good sexual health has been very important. Just like the mouth, the vagina links to important organs inside the body. For this reason, women are strongly advised to try as much as possible to maintain healthy sexual health to ensure optimal survival during their time on earth.







