Article Insights & Reflections
Synopsis: This report explains how legacy warnings and outdated interpretations still shape access to care. It summarizes current evidence, policy debates, and the reforms that could improve outcomes for women.
Top 5 Questions Answered:
- What did past studies like the WHI actually find?
- Which warnings are outdated and why?
- How do policies affect access to safe therapies?
- What does current evidence say about HRT safety?
- How might guideline changes improve care?
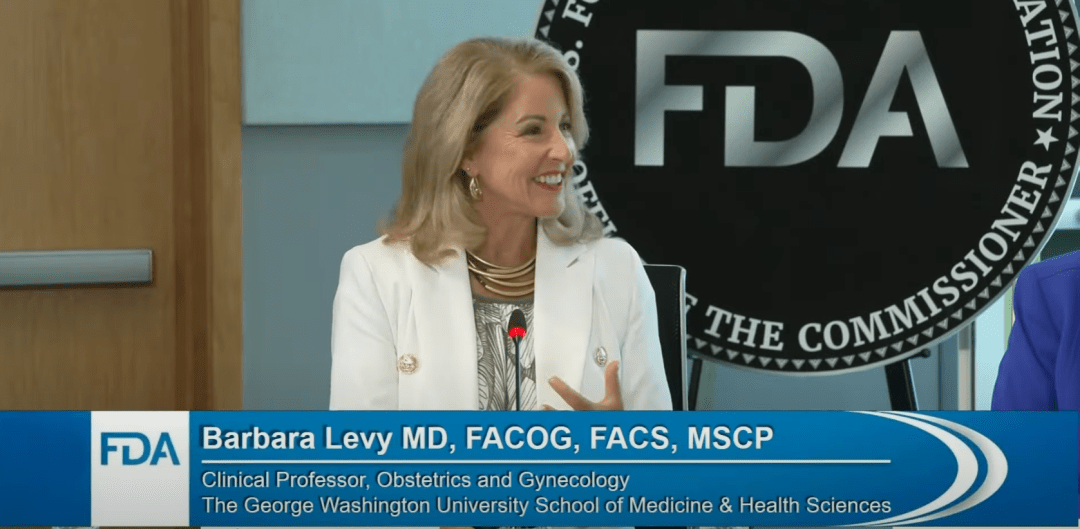
Dr. Barbara Levy, a renowned gynecologist and specialist in women’s health, spoke with urgency about the need to update FDA warnings on hormone therapy for menopausal women. Levy outlined how the now-infamous black box warning, which was attached after the Women’s Health Initiative (WHI) study in 2002, continues to limit access to HRT despite significant advancements in science and practice since that time.
Opening with an explanation of the origins of the black box warning, Dr. Levy described how the studies underpinning it used older formulations (such as conjugated equine estrogens and medroxyprogesterone acetate)—medications that differ substantially from the estradiol-based therapies more commonly prescribed today. She spotlighted the lack of differentiation between systemic and local (vaginal) hormone therapies in FDA warnings, arguing that this “one-size-fits-all” caution disregards both pharmacological science and contemporary clinical evidence.
Dr. Levy detailed newer research that links the timing and type of HRT to its risk-benefit profile. She emphasized that starting hormone therapy within 10 years of menopause onset—or before age 60—confers marked reductions in heart disease and osteoporotic fractures, with effectiveness comparable or superior to statin therapy for these endpoints. Such protective benefit does not extend to therapies initiated years after menopause. Importantly, Levy cited consistent findings that low-dose vaginal estrogen products, approved for urogenital symptoms, demonstrate no increase in cancer, stroke, or cardiovascular events, yet remain stigmatized due to class-wide labeling.
During her presentation, Dr. Levy analyzed the regulatory environment in the U.S. versus other countries, pointing out that many peer nations have approved and appropriately labeled hormone therapies for decades with no evidence of increased population risk. She highlighted how fear and regulatory inertia have driven U.S. physicians and women to avoid therapy that could dramatically improve quality of life, contributing to an epidemic of untreated menopause symptoms and excessive use of alternative, often unproven, remedies.
Perhaps most compelling was Dr. Levy’s critique of the professional landscape, where only about a third of training programs ensure menopause education for physicians. This, in her view, further entrenches outdated clinical habits built on past fears. She called on the FDA to create distinct pathways for local versus systemic hormone products, support evidence-based education for providers, and promote patient-centered decision making.
Dr. Levy closed with an appeal to logic and empathy: “It is time to move beyond the WHI. Women deserve counseling and access that is based on current science and their individual needs, not regulatory relics from another era.”