Reaching the age of menopause is a milestone worth celebrating as an aging woman. You would undergo bodily changes during and after the period and need to adjust. And these changes may not be all that likable.
Perimenopause (the period just before menopause) and menopause are the stages that mark the end of a woman’s reproductive years. These periods are, of course, a phase every woman would go through when the time comes. The age from which perimenopause and menopause symptoms are experienced ranges from about 40 to 65 years.
These periods related to hormonal changes can be linked with increased vulnerability to some diseases. Yeast or candida infection, for example, is more likely to be gotten in menopause. How true or probable is this?
Table of Contents
- What’s a candida infection?
- How can menopause cause candida infection?
- Common symptoms of the candida infection one might experience.
- Three forms of candida infection as classified by the Centers for Disease Control and Prevention.
- Top 5 common causes of candida overgrowth during menopause
- 10 Natural treatments for candida overgrowth
- How to reduce the risks of a candida infection even during menopause
What’s a Candida Infection?
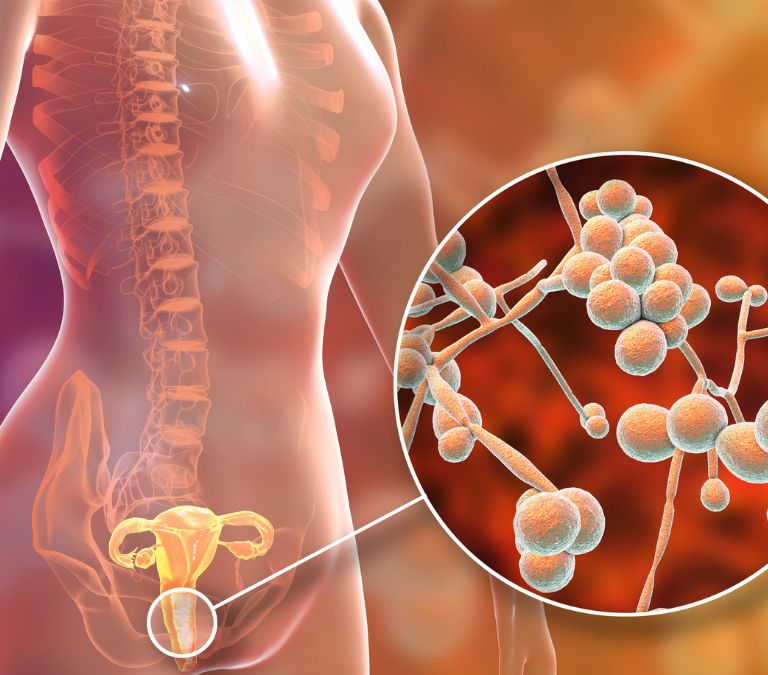
Candida infection is also known as yeast infection or candidiasis. It is a fungal disease on the body’s skin surfaces or the mucus membranes caused by the overgrowth of a yeast fungus called candida.
Candida fungus, just like many other fungi or bacteria in the body, lives in the body on surfaces like the mouth, vagina, throat, or mere skin without causing any harm. However, when the fungus multiplies and becomes an overgrowth, it poses a problem, leading to a candida infection.
How Can Menopause Cause Overgrowth of Candida?
Candida fungus can be found in and on the body. However, it is kept at harmless levels by acidic pH concentrations of the body fluids. The medium becomes less acidic if these pH balances are out of place. Then, fungi or other microorganisms can begin to grow and multiply in separate regions, causing an infection.
During menopause, your body undergoes many hormonal changes involving periods of sharp rises and falls in estrogen levels. It can cause an imbalance in the acidic levels, increasing the risk of a candida infection.
Symptoms of Yeast Infection
Many body symptoms often accompany candida infection and might help you realize an onset of the disease quite early on.
Itching and irritation of the vaginal area
Candida infection in the female genital area mostly has symptoms of itchy sensations and irritation of the vagina and vulva.
This itching can be a big problem if the candidiasis is left untreated for a long while. It can be pretty embarrassing, too – feeling the need to scratch your genital area almost every time.
Rash
One may also notice rashes develop around the affected area, especially if it’s a skin surface or vaginal area. Yeast infection rashes often look red and sharp with flat and scalloped edges.
These rashes are often itchy and painful, worsening the itchiness one is already dealing with. The infection rashes also give a hot sensation that can leave one feeling very uncomfortable in the affected area for the rest of the day.
Weakness or fatigue
A subtle symptom of candida infection may also be a feeling of tiredness or fatigue. A yeast infection is often due to the overgrowth of fungus permitted by an already weak immune system.
So, if the immune system is weak, the body may experience fatigue and weakness symptoms.
Watery discharges
Thick or watery vaginal discharges may also result from vaginal yeast infection. The discharges may be in the form of a thick, odorless and whitish fluid or a clear watery discharge.
However, this discharge would be different from any other normal discharge from the vaginal area. It’s also usually accompanied by the uncomfortable sweeping redness and itching of the vulva.
Pain or soreness
One might undergo soreness and pains in the moral tract due to scars or internal swellings if it’s oral thrush or oesophageal candida infection.
Vaginal candidiasis also causes painful and sore sensations in the genital areas worsening the discomfort characterized by the fungal infection.
Skin and nail fungus infection

Yeast infections may also manifest on the skin and fingernails and any other affected external body surface if that’s the area the fungal overgrowth populated. These areas are mostly very exposed, making it a very embarrassing situation to deal with.
Antifungal lotions and skin treatments can help, though, in this case.
Burning sensation during intercourse or urination
A woman with a vaginal yeast infection may also experience uncomfortable burning and painful sensations from her vagina during sexual intercourse or when urinating. It is mainly due to the soreness and lesions in the vaginal wall.
Redness or swelling of the vagina
Another general symptom is the redness of the vulva and vaginal wall. The vaginal wall may appear cracked and swollen in severe cases, mostly chronic.
Oral thrush
Oropharyngeal candidiasis is most often accompanied by symptoms of oral thrush and inflammation of the mouth, gut, or esophagus. It can develop into other symptoms like difficulty swallowing or loss of taste when eating or drinking.
Digestive issues
Invasive candidiasis in the stomach or intestines may mess up digestive functions and cause complications like bloating, indigestion, or ulcers.
Three Forms of the Candida Infection As Classified by the Centers for Disease Control and Prevention
Invasive Candidiasis
Invasive candidiasis is a form of candida infection that can develop into a severe infection affecting the heart, brain, blood, bones, eyes, and many other delicate organs.
This form of candidiasis is mainly a result of the multiplication of the microorganisms in the throat, mouth, esophagus, or on your skin surface. If the fungi find their way inside, especially into the bloodstream, this can lead to a candidiasis problem.
Since invasive candidiasis primarily manifests on the internal organs, it is not a contagious form of candida infection. Symptoms are hard to diagnose since they may be linked to many other medical conditions, but the most common symptoms include fevers and chills.
Candida infections of the Mouth, Throat, and Esophagus
This form of candida also occurs when the fungus found on the skin surfaces, mouth, throat, gut, etc., develops in unhealthy numbers. In this form, the fungal infection manifests in the oral areas like the mouth, throat, and esophagus.
When the infection affects the mouth and throat, it is called oral thrush or “oropharyngeal candidiasis.” In contrast, the candida infection of the esophagus is called esophageal candidiasis.
Symptoms may include white patches in the mouth, palates, on the tongue, and inner cheeks, pain during swallowing, or even loss of taste while eating.
Vaginal Candidiasis
Vaginal candidiasis, also called “vaginal yeast infection,” is the form of candidiasis women often have. It is most common during female hormonal fluctuations, like in menopause.
This form of candida infection results from the growth of the candid fungus found in the vaginal and genital areas. The imbalance of the female hormone estrogen can vary the pH balance too in the vagina. This pH change can cause the fungus to overgrow in harmful quantities, causing candida or yeast infection.
Symptoms of the vaginal yeast infection may be as mild as itching, soreness, or discomfort or severe, though rarely, like cracks and lesions in the vaginal wall.
Top 5 Common Causes of Candida Overgrowth during Menopause
It is safer to say that candidiasis isn’t necessarily contracted as a disease. Instead, it develops, and that is because the fungus isn’t gotten just before the infection exists. It has always been present but in harmless populations and conditions.
So, the causes of candida infection here refer to what makes the fungus multiply into overgrowth during menopause.
Hormonal Imbalance
Hormonal imbalance is the leading cause of yeast infection in women. The peaks and drops in the body’s estrogen levels create an unsteady balance for the optimum pH that should keep the fungus growth in check.
Hence, a yeast infection is likely to develop during hormonal changes like pregnancy, menopause, and the period just before menstruation.
Use of antibiotics
One of the microorganisms that can also be found in considerable amounts in your body is bacteria. And most of them can be called “good bacteria” because they are either unharmful or valuable to us for a particular purpose in the body.
A balance between the population of good bacteria and the candida fungus in the body also contributes to keeping the fungus growth in check.
When a woman takes antibiotics too often or without proper prescriptions, these can destroy some healthy bacteria, disturb the balance, and lead to an overgrowth.
Oral contraceptives or hormone therapy
In most contraceptive methods, you may use female estrogen to perform their functions. It can cause the female body to produce more sugar that encourages the growth of fungi.
Hormone therapy also allows more hormones in the body than needed. Taking in these hormones can lead to overgrowth by disturbing the balance of body hormones that keeps candida levels low.
Impaired Immune system
The immune system is essential in stopping infections and keeping candida out of the way. However, when the immune system is weak or damaged for any reason, the unwanted fungi can multiply and develop to unhealthy levels, causing candidiasis.
Eating foods that enhance the immune system, like fruits and veggies, should help.
Uncontrolled diabetes
Diabetes is a medical condition closely associated with high sugar levels in the body and manifests in the blood and even sweat, saliva, or urine.
And, of course, yeast loves to grow when sugar levels are high, so the medical condition becomes a bedding ground for the candida fungus.
10 Natural Treatments for Candida Overgrowth
Probiotics
Probiotics are medical supplements or drugs that do the opposite of what antibiotics do – they promote the growth of body bacteria, often good bacteria.
And these bacteria, in turn, help prevent an overgrowth of the fungi.
Be sure to take probiotics at the doctor’s prescription, though, so you don’t end up causing too many bacteria to grow, which might pose medical issues.
Stress management
Stress build-up also significantly promotes an overgrowth of the candida fungus. So, reducing stress to a bare minimum would help keep a candida overgrowth out of sight.
Stress upsets the balance of hormones and other ideal conditions and can trigger a fungal overgrowth.
It would help if you indulged in regular and effective stress management to avoid or treat a candida infection or mild overgrowth.

Boric acid
Boric acid has always proven helpful and is recommended by doctors to treat candida overgrowth. The acid can be used as a vaginal suppository.
Boric acid works to cure candidiasis by containing the growth of the candida fungus and making the environment unfavorable for an already existing overgrowth to thrive. The acid helps restore balance and maintain a healthy acidic vaginal pH and thus helps keep the fungal population in check.
Vitamin C
The immune system must be strong enough to work as the body’s primary defense against illnesses.
When a candida overgrowth occurs and a yeast infection is about to set in, a sound immune system would fight off the infection, acting as a last resort and keeping the body healthy.
Vitamin C is the most important to the body in strengthening the immune system, so regular intake would help prevent and fight against overgrowth.
Making dietary changes
Certain foods and drinks tend to make conditions more favorable for yeast to thrive, especially foods high in sugar.
So, if you are experiencing overgrowth or infection symptoms, try adjusting your diet to include fewer high-carbs or sugary foods.
Coconut oil
Another natural remedy to candida overgrowth is coconut oil.
Coconut oil is a well-known antifungal substance. It contains a medium-chain length fatty acid called caprylic acid. This caprylic acid effectively ruptures, kills off the yeast cell, and represses further fungal growth.
You should use this method less often, as it is yet to be certified as a recommended alternative to other common antifungal prescriptions.
Tea tree oil
Studies have shown that tea tree oil is another substance effective as an antimicrobial and antifungal substance.
It contains a necessary compound, terpinen-4-ol, which helps fight against and eliminate the candida fungus.
Garlic
Garlic and its extracts also have antifungal effects that prove helpful in dealing with candida fungus overgrowth.
Garlic contains an allicin ingredient that naturally fights off the candida fungus.
However, you shouldn’t insert garlic into the vagina directly. Many experiences of women who have tried such during candida symptoms have shown that it has adverse side effects.
It is better and ideal to apply it for oral thrush or use it as a food ingredient instead.
Natural Yogurt
Natural yogurt is also a probiotic as it helps good bacteria that can fight off a fungal overgrowth to grow. You can take this natural yogurt into the body through different means – orally or even by applying directly to the affected part.
Most people who have used this method usually report feeling rid of symptoms.
Get enough sleep too

Yes, it’s important to mention that sleep too is essential in dealing with candidiasis.
First, yeast infections can be caused or worsened by stress and inadequate rest.
The body constantly works to repair and maintain itself in a healthy state, and you can do your best to help it achieve that in any way you can.
Lack of rest and sleep will also contribute to hormonal fluctuations, a significant cause of candida overgrowth, so try to sleep well.
How to Reduce the Risks of Candida Infection even during menopause
Even though menopause is unavoidable for every woman, there are specific measures and practices you can indulge in to prevent the overgrowth o the candida fungus in your body parts. Thus, you can reduce the risks of contracting the infection even when menopause has made it more likely.
- Avoid tight-fitting clothing and underwear, especially non-breathable cotton underwear. Stick to loose and more unrestrained clothes.
- When cleaning after using the restroom, wipe from front to back instead of back to front to prevent carrying harmful microorganisms to the vaginal area.
- Maintain overall personal hygiene. Avoid using unclean materials around the genital areas and change pads and tampons regularly.
- Avoid taking unnecessary and unprescribed antibiotics. These antibiotics can potentially kill helpful bacteria in the body, which are essential to maintain the fungi levels in the body and prevent overgrowth.
- Always dry the genital areas thoroughly after a bath or swim. Also, avoid wet articles of clothing around the genital area.
Conclusion
Menopause comes with its challenges, medically and otherwise, and it’s up to you as a woman to manage yourself properly at that stage of life. If you do it right, menopause should not pose much of a problem to you, especially with yeast infections.
Candida infection in itself is not a severe condition, and most of the time, a woman may have overgrowth or an infection, maybe once or twice in a lifetime. It hardly develops into a severe medical case.
However, that does not make it any less unpleasurable, and you want to avoid it as much as possible.
You now have virtually everything about menopause and its relation to candidiasis. So, whether you are a woman already in menopause, about to undergo menopause, or already experiencing some uncomfortable symptoms related to aging or menopause, or not, you have what you need in this article. The ball is now in your court to keep the doctor away!
Frequently Asked Questions
Are yeast infections sexually transmitted?
Candida infection is, by definition, not a transmitted disease. However, the risk remains that it might be contracted by an uninfected person if they have unprotected sex with an infected person – though very rare.
Doctors advise against having sex when battling yeast infections until the symptoms are well cured.
The risks of transmitting candidiasis during intercourse also vary depending on the involved. It is infrequent for men to have the disease (and even rarer for circumcised men); hence, the transmission, if it occurs at all, is mostly from woman to man. Same-sex intercourse, too, between women increases the likelihood.
Having sexual intercourse while experiencing yeast infection is also uncomfortable due to the painful symptoms the infected partner might experience.
Can vitamins help in preventing yeast infections?
Vitamins and supplements play significant roles in curbing the overgrowing of yeast fungi in the body. Vitamins like Vitamin B6 and Vitamin D help control candidiasis, and vitamin C is also essential to strengthening the body’s immune system to fight off the infection.
Does menstruation make yeast infections more likely?
A woman’s menstrual period is a period of high estrogen production levels in the female’s body. Since high amounts of hormones are in circulation in the body, the pH balance tends to be more acidic and hence, does not give optimum conditions for overgrowth of the Candida fungus. So, the chances of having yeast infections during menstruation are significantly lower.
However, the periods just before the menstrual period are characterized by deficient levels of estrogen hormones. The fungi may overgrow, and yeast infections can occur in that period.
Can certain foods cause candida infection?
Yeast is a fungus that thrives on food substances like high sugar and alcohol, so eating high-sugar foods or foods with many carbs might trigger an overgrowth of the fungus. Alcoholic drinks, too, may set off or worsen the situation.
Therefore, healthy practice for reducing the risk of candida infection or treating the disease is to make dietary changes making less accommodation for foods that favor the growth of the yeast fungus.
How does pregnancy affect candida overgrowth?
Pregnancy is the period in a woman when she’s most susceptible to yeast infections. Why is this so? Pregnancy is characterized by hormonal fluctuations with different estrogen hormone levels in circulation.
It results in the upsetting of the acidic balance in the body, and yeast fungi are no longer kept in check and tend to multiply over time.
This medical situation needs to be looked out for during pregnancy as yeast infections can be passed to the baby and lead to some medical complications.







