Article Insights & Reflections
Synopsis: This overview brings clarity to a key menopause topic and translates research into practical next steps. It equips readers with options to discuss with a qualified clinician and tools to start improving today.
Top 5 Questions Answered:
- Which symptoms are truly driven by menopause?
- What options exist beyond over-the-counter fixes?
- When should I consider medical therapy?
- Which daily habits make the biggest difference?
- How do I personalize a plan that lasts?
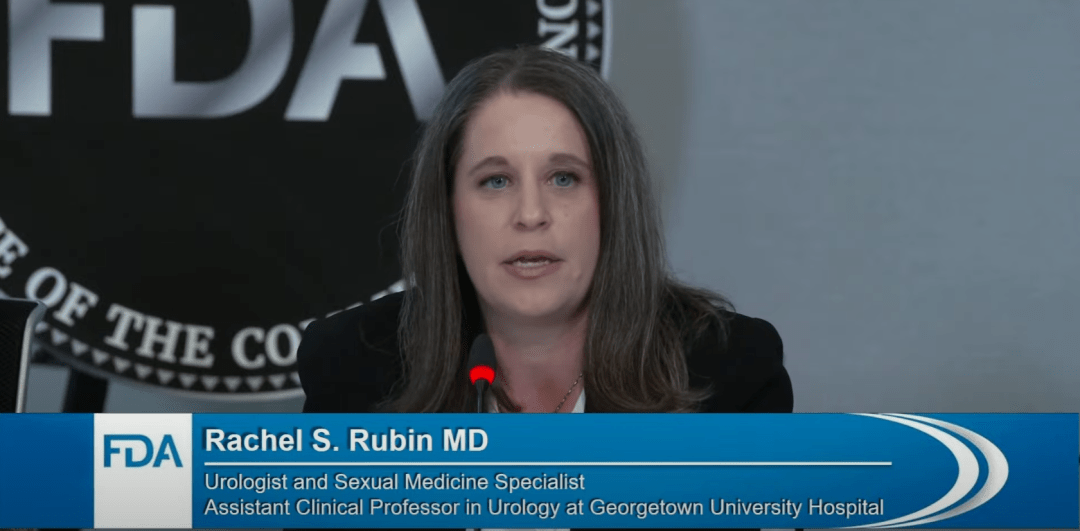
Dr. Rachel S. Rubin, fellowship-trained urologist and sexual medicine expert, used her time to elevate the discussion around genital and urinary syndrome of menopause (GSM). She shared the historical context of how the understanding of urogenital symptoms evolved, with advocacy shifting policy language toward a whole-system view of menopause.
Dr. Rubin delved into the specifics of genital and urinary tissue—highly estrogen-sensitive yet neglected for decades in research and clinical care. She highlighted the microbiome’s dependence on estrogen, tying this to increased urinary tract infections, sexual pain, and compromised bladder function in untreated menopause.
Rubin presented compelling economic arguments, noting that the costs associated with preventable complications far exceed investment in safe, evidence-backed local hormone products. On a population level, she explained, broader access to vaginal estrogen would mean fewer hospitalizations, specialist consults, and lost productivity—translating into both improved health and national economic benefit.
She concluded by urging the FDA to overhaul its warnings in line with global standards and current scientific understanding, to reduce unnecessary fear and improve access to care for millions.