Menopause is a natural and difficult stage of life. Progesterone or hormone replacement treatment (HRT) can help to alleviate the severe symptoms that hormone changes cause, even while changes in hormone levels are not prevented.
Your body’s production of the hormones – progesterone, estrogen, and testosterone, is significantly reduced during perimenopause. Eventually, menstrual cycles will also end entirely. You need to know that menopause has its gains and pains.
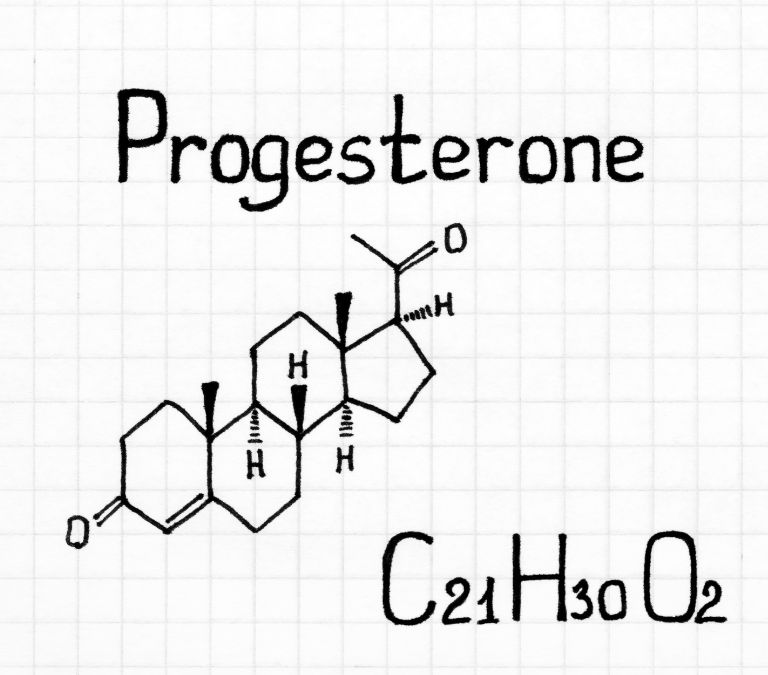
The corpus luteum of the ovaries produces progesterone, a transient gland that develops after the ovary releases an egg. The placenta and the adrenal glands can also produce progesterone. Progesterone’s primary role in the female body is to control menstruation and aid in pregnancy.
Ovulation occurs in the middle of a person’s menstrual cycle when luteinizing hormone levels rise. The process of releasing an egg from one of your two ovaries is called ovulation. The corpus luteum develops and starts generating progesterone once the egg is released.
After ovulation, progesterone peaks, either staying high if you become pregnant or decreasing if you do not. Your uterine lining will then start to release due to this hormone decline.
Progesterone is essential for healthy conception and pregnancy, but it is also vital whether you are attempting to conceive or not.
Benefits of Progesterone for Mood, Anxiety, and Depression
You might be surprised to learn that progesterone has antidepressant properties and can improve your mood and reduce anxiety. It activates the “feel-good” region of the brain. As a result, when progesterone levels fall during menopause, anxiety can become a primary menopausal symptom. Studies have found that progesterone is the hormone for menopausal women with the most anti-anxiety effects.
The major reason for moodiness, brain fog, and sadness following menopause is a progesterone hormone deficit, despite many other causes of worry, such as your kids, work, or anything else. Some potential advantages of progesterone for postmenopausal symptoms include the following.
- Fewer night sweats and hot flashes
A recent research discovered that progesterone reduced hot flashes and nocturnal sweats in typical postmenopausal women. They were also less severe when they did encounter them.
- Better sleeping ability
The use of progesterone at night improves your sleep. According to a 2018 study, taking 300mg of progesterone before bedtime caused people to sleep for longer nights and have fewer night sweats.
- Reduces brain fogginess
Many women have brain fog as a menopausal symptom, and progesterone may be able to alleviate this. For instance, a 2015 study discovered that progesterone enhanced patients’ verbal and visual memory. But other researchers haven’t produced the same outcomes.
After ovulation, progesterone aids in uterine lining (endometrium) preparation for a future pregnancy. Additionally, by preventing the uterus from tightening, this hormone reduces the risk of the body rejecting a fertilized egg. Progesterone stimulates the body to sustain the endometrium, which feeds the developing fetus, throughout pregnancy. Additionally, this hormone encourages the body to begin producing breast milk.
Progesterone-based hormone replacement treatment can be a useful way to treat typical postmenopausal symptoms, including hot flashes and night sweats. Progesterone after menopause has additional advantages, including its capacity to alleviate additional symptoms like:
- Vaginal signs, such as dryness, itching, and burning.
- Osteoporosis (which leads to bone loss and fractures).
- A heart attack and a stroke.
- Bipolar tendencies.
- Anxiety and Depression.
According to researchers, progesterone may offer several other advantages after menopause.
To lessen menopausal and postmenopausal symptoms, you should add progesterone to many hormone replacement therapies, even though estrogen is frequently the main component.
If your uterus is still there, this is particularly true. Endometrial hyperplasia, or an excessively thick uterine lining, is prevented by progesterone by helping to shrink the uterine lining. By doing this, the chance of getting uterine or endometrial cancer is decreased.
Benefits of Progesterone to Women
Progesterone helps the body to prepare the uterus for pregnancy by thickening the endometrial lining. It is impossible to maintain pregnancy if this doesn’t happen because of low progesterone levels or if levels don’t increase after the egg implants.
Women experience perimenopause as they go from their reproductive years into menopause. Progesterone and other hormone levels start to decline during this period. Women may experience irregular or heavy periods as a result, and they may also have trouble falling asleep. Bioidentical progesterone replacement therapy can lessen or possibly cure these symptoms.
Many people refer to progesterone as the miracle hormone. Both the body and the brain are calmed by it. Lower levels can result in irregular moods, elevated anxiety, and sadness. Because progesterone is a neuro-steroid, it enhances typical brain functions and supports healthy nervous system operation. Since bioidentical progesterone has a calming effect and can help restore regular sleep cycles, we advise taking it before bed. Supplementing with progesterone has additional advantages listed below.
- It decreases fear
- It enhances memory
- It can help prevent breast or the uterus cancer
- It aids the prevention of uterine lining cell proliferation and the development of endometriosis
- It reduces the risk of ovarian and fibrocystic disease
- Helps with the symptoms of PMS.
- It stops the buildup of plaque on arterial walls
- Enhances libido and improves slumber
- It cures or reduces Migraines
- Improves the capacity to handle stress and aids in using fat for energy.
- It is essential for the development of bones
- It aids the thyroid gland’s optimal operation
- It can aid the anti-aging process
- It reduces joint pain and inflammation
- It regulates menstrual cycles
- Prevents excessive weight gain
Your body creates a variety of hormones that interact with one another like instruments in a symphony. Progesterone is only one of these hormones. One hormone’s imbalance or deficiency can have an impact on others. Therefore, estrogen and progesterone cooperate to help your body function normally.
What Happens to Every Woman’s Hormone Levels during Menopause and Postmenopause?

Your body naturally goes through the menopause phase. You might not require any menopausal therapy in some circumstances. When considering menopausal treatment with your doctor, focus on addressing the symptoms that interfere with your daily life. You can treat the symptoms of menopause in a variety of ways.
Your body experiences significant hormonal changes and produces fewer hormones during menopause, including progesterone and estrogen. Progesterone and estrogen ovaries generate these hormones. Hormone treatment can be used as a supplement when your ovaries cannot produce enough estrogen and progesterone.
The body uses hormones as messengers to speed up, slow down, and start or stop physical and chemical processes in all bodily systems. Hormones flow through the bloodstream. The two hormones that regulate the reproductive system, including the menstrual cycle and female fertility, are produced by your ovaries: estrogen and progesterone.
You have all the eggs you will ever have when you are born. The follicles in the ovaries are where the eggs are located. The quantity of ovarian follicles decreases, and the ovaries become less receptive to the two additional hormones involved throughout menopause.
Luteinizing hormone (LH) and Follicle-stimulating Hormone (FSH) are released during pregnancy (FSH). Hormonal changes may negatively impact your health for years due to these unavoidable hormonal changes and the normal fall in estrogen levels that occur throughout menopause.
During your midlife years, the amounts of other hormones produced by the ovaries, such as progesterone and testosterone, a male androgen hormone produced at lesser levels in women), are also shifting.
Menstrual cycles are more affected by progesterone fluctuations than sexual function. However, age-related testosterone losses may reduce libido (sex desire) in middle-aged women, but this is still debatable. Some people think libido shouldn’t decrease after menopause because estrogen lowers more than testosterone. Women’s testosterone levels fall years before perimenopause and are exclusively age-related, not menopause-related.
The years between a woman’s reproductive years and menopause are known as the menopausal transition (perimenopause). If a woman has gone a full year without having a period, she is considered to be in menopause. When a woman enters menopause, her ovaries effectively stop producing hormones, which makes it impossible for her to get pregnant. Menopause typically occurs around 51 years old. Each woman’s perimenopause is unique, although it typically lasts five years.
Low progesterone can result in irregular, prolonged, and heavier periods during perimenopause. Infrequent menstrual periods, vaginal dryness, hot flashes or flushes, and sleep issues are common during the menopausal transition. While some of these symptoms are constant, others are temporary. The symptoms might interfere with everyday activities and range from minor to severe.
Hormonal Changes That Happen as Menopause Approaches
Changes in hormone levels cause many symptoms you experience throughout the transition. Hot flashes, vaginal dryness, and changes in the menstrual cycle and sleep patterns can all be brought on by these adjustments. Together, hormones help maintain equilibrium. The ovaries or pituitary glands in the brain produce more or less other hormones in response to changes in hormone levels. The hormonal balance in a woman varies as she ages.
Follicle-stimulating Hormone (FSH)
The pituitary gland produces FSH. Throughout the menopausal transition, levels frequently rise and fall. FSH levels might fluctuate greatly from one day to the next. The ovaries produce more estrogen when FSH levels are elevated. Estrogen levels decrease as FSH levels do. FSH and estrogen levels can vary months to years before menopause.
Inhibin
A reduction in the hormone inhibin is one of the early hormonal changes. Inhibin is produced by the ovary and signals the pituitary gland to produce fewer follicle-stimulating hormones (FSH). FSH levels increase when inhibin levels decrease. Years to months before a woman starts the menopausal transition, the blood levels of these hormones might alter.
Progesterone
Ovarian progesterone production rises following ovulation (release of an egg from the ovary). A woman’s progesterone levels might stay low when she ovulates less frequently. resulting in a missed menstruation.
AMH
Like inhibin, antimüllerian hormone (AMH) is produced by the ovaries. A woman’s AMH levels decline with age and become unnoticeable a couple of years before menopause.
It’s critical to realize that every woman experiences hormonal fluctuations differently. No particular blood test can predict or diagnose a woman in the menopausal transition, even though high FSH and low AMH and inhibin levels are frequently observed in this stage.
Top Sources of Progesterone

Your body naturally produces progesterone, but progestin hormone is a term for progesterone-like substances that scientists have developed to mimic the effects of progesterone. It indicates that progestin is artificial.
Low progesterone levels or hormonal imbalances can be treated using synthetic progesterone or bioidentical Progesterone. Since many individuals consider these products to be safer alternatives to taking natural progesterone, they have grown extremely popular over time.
Various kinds of bioidentical progesterone exist. Some are custom-made in pharmacies using a technique known as compounding, while others are pre-fabricated by pharmaceutical corporations. Pre-made medications have the advantage that numerous have.
However, some of the top food sources of progesterone are:
- Dark Chocolate
Dark chocolate is another item that raises progesterone levels. Magnesium is present in dark chocolate, and as previously mentioned, because magnesium may reduce estrogen, this can have a very positive impact on total progesterone.
- Poultry
Common poultry sources that enhance progesterone include chicken and turkey. These are abundant in vitamin B6. These lean meats enhance progesterone because they are high in vitamin B6, which is present in abundance. Water-soluble vitamin B6 is crucial for supporting the reproductive system.
- Nuts
Nuts are excellent progesterone sources due to minerals, zinc, and magnesium.
An essential mineral called zinc is used to support the reproductive system. According to research, zinc can enhance the number of binding sites on a progesterone receptor, leading to higher amounts of total progesterone.
Magnesium is a mineral that aids in creating muscle protein, neuron function, and numerous enzymatic activities.
- Citrus
Citrus fruits are foods that enhance progesterone since they are a strong source of vitamin C. Water-soluble vitamin C promotes the production of scar tissue, aids in the healing of wounds, and helps to preserve skin integrity and tissue.
- Leafy Vegetables
Leafy vegetables are also helpful for increasing progesterone. These meals include magnesium and calcium, two elements that actively alter progesterone.
- Peppers
Citrus and peppers both have significant vitamin C content. Red peppers, in particular, offer the greatest vitamin C because they raise progesterone levels.
- Avocados
Avocados are one of the foods to raise progesterone since they include a lot of beneficial fats. Healthy fats are unsaturated, which means their fatty acid chains include at least one double bond.
- Salmon
One of the few meals, salmon, has high omega 3 fatty acids, a form of good fat known as polyunsaturated fats. Salmon is one of the meals that raise progesterone. As a result, LH, which is increased by omega 3 fatty acids, can also enhance progesterone production.
- Shrimps
Shrimp is another item that naturally raises progesterone levels. This protein is also lean, indicating that it has fewer fat calories than typical meat and is rich in zinc.
- Cruciferous Vegetables
Among the vegetables of the crucifer family are broccoli, cauliflower, and cabbage. Due to their ability to detoxify estrogen, these vegetables are regarded as one of the meals that might raise progesterone. Estrogen dominance, or a larger ratio of estrogen to progesterone, may cause low levels of progesterone in the body.
A Look at All Progesterone Delivery Methods
- SUBCUTANEOUS (under the skin) METHOD
The body responds to hormones because it is the most natural method. It behaves most closely with the ovaries and testicles. The body takes what it requires as it arises. Numerous patients choose this vehicle, and many doctors solely do this kind of HRT. For implantation, women should see their doctor every three to four months, and males every four to six months. You can have some minor bruising and will feel painful for three to four days. The operation is not at all painful. A stick is felt, followed by 3 seconds of burning.
- INJECTION (into the muscle with a needle)
Medroxyprogesterone acetate, sometimes Depo-Provera, is a prevalent form of this progesterone.
- TRANSDERMAL (absorbed through the skin)
This method will skip the liver and is the one patients choose the most. However, you must do this every day at the same time and make sure to cleanse the application site first. You apply the HRT lotion to the inner arms or upper inner thighs. To prevent saturation of the receptor site, you must rotate sites.
- SUBLINGUAL (under the tongue)
This procedure will bypass the liver. However, many patients complain that it tastes bad, and this option doesn’t always result in the highest patient compliance.
- ORAL (by mouth)
Any hormone treatment, including bioidentical HRT, should not be administered this way. This mechanism does not bypass the liver. Hence it has more effects on patients.
Other delivery methods include vaginal and rectal.
Is progesterone therapy Necessary after menopause?
Your estrogen levels decrease throughout menopause. Some women experience disturbing symptoms, including vaginal dryness and hot flashes. The most effective and common treatment for menopause symptoms is Hormone Replacement Therapy, also referred to as hormone therapy, menopausal hormone therapy, and estrogen replacement therapy.
Compared to estrogen alone, taking estrogen and progesterone decreases your chance of developing endometrial cancer.
Progesterone can assist in alleviating menopausal symptoms, such as hot flashes, despite being typically used as a birth control method.
How much progesterone should postmenopausal women take?
- The hormone replacement treatment (HRT) should be 200 mg micronized progesterone (Prometrium) each day, and 0.625 mg conjugated estrogens, commonly given for 12 days out of a 25-day cycle. It applies to oral delivery methods.
- For menopausal symptoms, daily applications of 20 mg progesterone cream, equal to 1/4 teaspoon of progesterone cream, are commonly applied to various body parts, such as the upper arms, thighs, or breasts.
- Progesterone has been used to treat endometrial hyperplasia to reduce abnormal uterine lining thickness with doses of 90 mg (Crinone 8%), or 100 mg progesterone cream used intravaginally daily from day 10 to day 25 or on 2 days interval from the 17th day of a 28-day cycle.
Side Effects of Progesterone Therapy and How to Reduce Them
HRT has unfavorable side effects. Progesterone can have several negative side effects, including gastrointestinal distress, altered appetite, weight gain, fluid retention and swelling (edema), exhaustion, acne, sleepiness, allergic skin rashes, fever, headache, depression, sleeplessness, and discomfort or enlargement of the breasts. It is also extremely unsafe when used for any reason during pregnancy. The common negative effects of progesterone therapy are:
- Bloating
- Breast enlargement or sensitivity
- Headaches
- Mood swings
- Nausea
- Uterine bleeding
Prevention
The type and severity of the side effects depend on several conditions. The main factor is the dose. However, the side effects also depend on how progesterone interacts with your hormone receptors and how your body uses it.
The advantages of taking progesterone after menopause exceed the hazards for many women. You may also take many actions to lessen your chance of suffering negative side effects and health hazards from using progesterone for menopause.
- See the doctor as you need to determine the right progesterone supplement and administration approach.
- Use as little medicine as possible.
- Continue to visit your doctor for updates.
- Do not use progesterone if you have vascular disease.
- Refrain from using progesterone if you’re battling breast cancer unless your doctor instructs you to.
- If you often experience significant depression or have a history of experiencing major depression, see your healthcare professional before taking progesterone.
- Do not use progesterone if you have undetected vaginal bleeding.
Conclusion
The best way to address menopausal symptoms is to attempt natural hormone replacement therapy (HRT), which contains progesterone. It’s typical to only recommend estrogen therapy when a woman doesn’t have a uterus. The body may readily absorb progesterone in small amounts in pills or creams containing micronized progesterone.
If at all necessary, progesterone treatment should begin before menopause. It could be too late to begin progesterone therapy if a woman is above 60 or has been menopausal for more than ten years.