Women going through or getting close to menopause often worry about whether the symptoms they are experiencing are caused by menopause or by something else, like cancer. But some menopause symptoms may be like those of some types of cancer. Or does menopause or the treatment for it increase the risk of cancer?
You need to know how menopause and cancer symptoms are similar and how menopause may or may not increase your cancer risk.
What Is Menopause?

Menopause is said to have happened when the ovaries stop making eggs. If you haven’t had a period for a year, that’s usually enough proof (with no other obvious causes). On average, the age of menopause is 51, which usually starts when a woman is in her late 40s or early 50s.
The transition into menopause is called “perimenopause,” It can start up to eight years before menopause starts. The ovaries are making less estrogen and progesterone at this time. Because of this, the person’s menstrual cycles will become more irregular until they stop completely, and the body will undergo some changes. As this happens, menopausal symptoms caused by a hormone drop may show up.
Postmenopause is the time after menopause when some women say their menopause symptoms have lessened or gone away completely.
It’s important to tell the difference between the signs of menopause and those of gynecologic cancers, which start in the female reproductive organs. Cancers of the uterus, ovaries, and cervix are the most prevalent forms of gynecologic malignancy. To ensure that signs of a possible underlying malignancy aren’t ignored or misread as menopause symptoms, it’s important to know how they are similar and different.
Does Menopause Cause Cancer?
A woman’s risk of getting cancer increases as she ages, not when she goes through menopause. Due to their age, women who have gone through menopause are more likely to get cancer.
No medical rule says a woman should limit the number of times she ovulates to lower her cancer risk later. However, it is important to remember that getting older is the biggest risk factor for many types of cancer.
As you get older, your chance of getting cancer goes up. Age is the most important factor in getting cancer and dying from it.
The National Cancer Institute says that the average age at which someone is first told they have cancer is 66. Most women go through menopause at age 51. Delaying menopause could have health benefits like a longer life span and a lower risk of heart disease. But studies show that a woman’s chance of getting several types of cancer increases if she has more menstrual cycles.
Women going through menopause after age 55 are more likely to get breast and uterine cancer because they’ve been exposed to estrogen for longer. The chance of getting ovarian cancer is also a bit higher, probably because there are more ovulations.
During a woman’s period, estrogen is released into her body and can be found in her breasts and uterus. Also, a higher number of menstrual cycles over a woman’s lifetime is linked to a higher risk of breast cancer because of exposure to estrogen.
According to the research, multiple factors make someone more likely to get breast cancer. Your risk increases significantly if you are a woman or an older person. Most breast cancer is found in women over the age of 50.
Some women will get breast cancer even though they don’t have any known risk factors for it. Even if a risk factor is present, it doesn’t mean the disease will happen, and not all risk factors have the same effect. Even though many things put women at risk for breast cancer, the disease does not affect most women. If you have the risk of breast cancer, you should talk to your doctor about ways to prevent it and tests for it.
Possible Causes Of Cancer
- Aging.
Aging is the main reason why people get breast cancer. Most women are 50 when they are told they have breast cancer.
- Having a lot of breast tissue.
If your breasts have a lot of connective tissue, it might be hard to find cancer on a mammogram. Women are more likely to get breast cancer if they have larger breasts.
- A history of breast cancer or other breast problems in your family or yourself.
A woman who has already been diagnosed with breast cancer has a higher chance of getting it again. Atypical hyperplasia and lobular carcinoma in situ are two types of precancerous breast disease linked to a higher chance of getting invasive breast cancer.
- Changes in the way genes work.
Women who have inherited changes to certain genes are more likely to get breast and ovarian cancer.
- Having a breast or ovarian cancer-stricken mother, father, aunt, or sister.
If a woman’s mother, sister, daughter (first-degree relatives), or many people on either her mother’s or father’s side of the family have had breast or ovarian cancer, she is more likely to get it herself. If a woman has a first-degree male relative with the disease, she is more likely to get it herself.
- Changes in pregnancy hormones.
It is known that women are more likely to get breast cancer if they are exposed to hormones for a long time, like when their periods start before age 12 or if they don’t go through menopause until after age 55. Also, it has been shown that women who have their first child after age 30, don’t breastfeed, and have never carried a pregnancy are more likely to get breast cancer.
- Treatment with radiation therapy
Women who had radiation therapy to their chest or breasts before they turned 30 are more likely to get breast cancer.
Lifestyle Causes
-
Being Overweight: After menopause, it’s hard to stay at a healthy weight. Women over 50 who are overweight or obese are more likely to get breast cancer than women who are not overweight or obese.
-
Alcohol: According to scientific research, the more a woman drinks, the more likely she is to get breast cancer.
-
Taking hormones: Hormone replacement therapy (HRT) for menopause, which includes both estrogen and progesterone and has been used for more than five years, is linked to an increased risk of breast cancer. Several oral contraceptives have also been linked to an increased risk of breast cancer (birth control tablets).
-
Smoking: A higher risk of breast cancer has also been linked to smoking, exposure to chemicals that cause cancer, and changes in other hormones caused by night shifts.
-
Laziness: Women who don’t do as much work are more likely to get breast cancer.
Top Three Cancers Menopausal Women Are At Risk Of

- Breast cancer
Women are more likely to get breast cancer than any other invasive cancer. Also, it is the cause of a disproportionately high number of deaths from cancer in women.
With the help of modern ways to diagnose and treat breast cancer, the number of people who survive it has increased significantly. Between 1989 and 2017, the number of people getting breast cancer fell by about 40%.
But a study in 2019 suggested that the rate may have stopped rising among American women ages 20 to 39.
Symptoms Of Breast Cancer
- Lumps
Most of the time, the first sign of breast cancer is a lump or an area where the breast tissue has grown.
-
Pitting, or color changes, like redness, in the breast skin.
-
A rash around one nipple. Discharge from a nipple, which may contain blood. A sunken or inverted nipple.
-
Pain in the armpit or breast.
-
Breast enlargement or reduction.
-
Peeling, flaking, or scaling of breast or nipple skin.
Causes Of Breast Cancer
After a girl hits puberty, her breasts are made up of fatty tissue, connective tissue, and thousands of lobules. We’re talking about glands that make milk, and they’re pretty small. Through a chain of tiny tubes called ducts, the milk gets to the nipple.
When DNA gets changed or broken, it can cause breast cancer to grow. Some causes are exposure to estrogen, genes that cause cancer passed down through families, and genetic defects.
The immune system will look for abnormal cells or growths in a healthy body and kill them. When someone has cancer, none of these things happen. Because of this, breast tissue cells start to multiply uncontrollably and do not die off as they normally would. When cells multiply out of control, a tumor forms, which starves the healthy cells in the body.
The start of breast cancer typically begins in the lining of the milk ducts or the lobules that drain the milk into them. From there, it could spread to other parts of the body.
- Endometrial Cancer
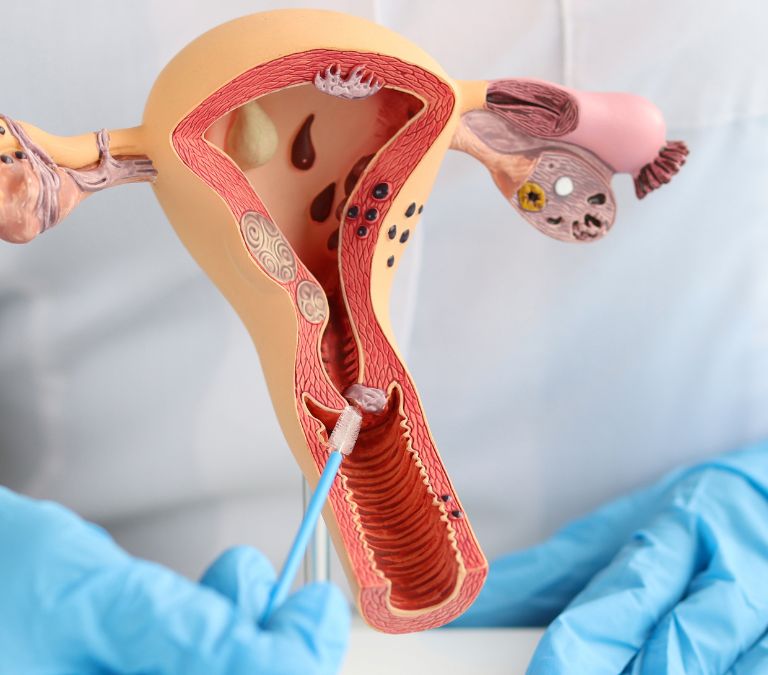
The uterus can be the site of the development of endometrial cancer. The uterus, shaped like a pear, is a pelvic organ that houses the developing fetus.
Endometrial cancer starts in the cells that make up the uterus lining, the endometrium. Endometrial cancer is a type of cancer that forms in the cells that line the uterus. Endometrial cancer is one of the types of uterine cancer. Uterine sarcoma is another type, but it is very rare.
Endometrial cancer is often found early because it causes abnormal bleeding in the uterus. Endometrial cancer is often treated by removing the uterus through surgery. If caught early, this can be a cure.
Symptoms Of Endometrial Cancer
-
Changes in hormones and bleeding from the cervix.
-
Heavy periods
-
Stomach ache
Possible Causes Of Endometrial Cancer
-
When your body makes more estrogen than usual but the same amount of progesterone, your risk of endometrial cancer increases. For example, polycystic ovary syndrome, obesity, and diabetes can cause ovulation at odd times.
-
Changes in a woman’s body affect how estrogen moves through her body. Progesterone and estrogen are two of the most important hormones the ovaries make for women. The endometrium adapts to changes in the balance of hormones.
-
Endometrial cancer risk increases when estrogen-only hormones are used after menopause.
-
The risk of endometrial cancer can also rise in uncommon ovarian tumors that release estrogen.
-
Women who have never given birth are more likely to get endometrial cancer than those who have.
-
Aging: Endometrial cancer risk rises with age. Menopause is associated with an increase in endometrial cancer.
-
Obesity. You’re more likely to get endometrial cancer if you’re overweight. Possible cause: hormone balance disruption brought on by carrying around extra pounds.
-
Endometrial cancer risk is increased by early menstruation (before age 12) and delayed onset of menopause. The more estrogen your endometrium has been exposed to, the more periods you’ve had.
-
Using hormones to cure breast cancer.
- Ovarian Cancer
Even though it’s called “ovarian cancer,” it doesn’t start in the ovaries. Instead, it starts in other parts of a woman’s reproductive system. But it happens more often in women over 50, though it can happen to anyone. The American Cancer Society says that half of all cases of ovarian cancer are found in women over the age of 63.
Menopause does not cause ovarian cancer. But as you grow older, your chance of getting it also increases. Menopause is a natural part of getting older, and as a result, it brings more risks.
Some things about menopause can make or break your chance of getting ovarian cancer.
Possible Causes Of Ovarian Cancer
-
Late menopause, usually in women over 52; This may be because you’re ovulating more often now. Menstruation is a hormone sign that it’s time to ovulate.
-
Taking birth control pills can stop you from ovulating for a short time. In this way, you can cut the chance of getting ovarian cancer. It would be a good idea to see a doctor. You may be less likely to get cancer if you take birth control pills, but you must weigh this against the fact that they may cause other problems.
-
Women often use hormone therapy to deal with menopause symptoms such as hot flashes and bone loss. Some findings have found a link between these hormones and a higher chance of getting ovarian cancer.
Progestin is a synthetic hormone that is used in hormone replacement therapy. It can be taken alone, with progesterone, or in place of progesterone. The American Cancer Society says that if you take estrogen without progesterone for a long time (at least 5 or 10 years), you may be more likely to get cancer.
Symptoms Of Ovarian Cancer

For a long time, the term “silent disease” was often used to describe ovarian cancer. If you know the signs, your doctor will likely find it early. Women often find out they have ovarian cancer after it has already spread to other body parts; it’s often very hard to get better.
When menopause starts, it is important to know the signs of ovarian cancer. Some symptoms are constipation, bloating, swelling, pain in the pelvis, and weight loss.
Typical Symptoms Of Ovarian Cancer
Most of the time, there are four different signs of ovarian cancer. You may already have them in the early stages of the disease. These signs are:
-
An ache in the lower abdomen or pelvis
-
Feelings of hunger that don’t go away or feeling full quickly
-
Having a strong urge to urinate always or the need to urinate often.
-
Bloating
There are many things besides ovarian cancer that can cause these signs. You can only worry if they are unusual for you and if they are getting worse or happening more often.
Other ovarian cancer signs and symptoms
-
Fatigue
-
Pain during sex
-
Back pain
-
Feeling sick
-
heartburn
-
Constipation
-
Changes in weight
-
Unusual spotting or bleeding from the uterus, especially after menopause
Remember that these things could be signs of ovarian cancer but may also be caused by something else.
Early Menopause Caused By Cancer
As a result of their treatment, women with cancer often start menopause early. If a woman stops taking hormone replacement therapy, goes through chemotherapy, or uses hormone therapy, her menopause symptoms can return.
Even though there are differences in how each woman responds to treatment, some negative effects are common.
Cancer Treatments That Can Cause Early Menopause
Cancer treatments have been linked to some women going through menopause before they should have. When a woman goes through menopause before she turns 40, it means that her ovaries have stopped making eggs, so you can’t get pregnant or have periods.
If you go through menopause too soon, you might have hot flashes and a dry uterus, among other things. If you have these symptoms, you should speak to a doctor about how to treat them.
Here are some cancer treatments that can cause menopause to happen earlier than usual:
- Surgery.
When both ovaries are taken out, menopause starts right away. If you are under 50, your doctor may decide to keep at least one of your ovaries. It can keep you from going through menopause before you should.
- Radiation.
The ovaries are also at risk when radiation is sent to the pelvic area. Your ovaries might be able to heal and start making eggs again. But a lot of radiation exposure could have long-term effects.
- Hormone Replacement
Hormones are used as part of medical treatment. Often, the side effects of breast and uterine cancer treatments can cause menopause to start earlier than expected.
- Chemotherapy (chemo)
Depending on your chemotherapy, the damage to your ovaries could cause you to go through menopause early. Menopause can happen quickly, or it can take months after treatment. How likely you will go through menopause early because of chemotherapy depends on how much and what kind of chemo you are getting. If you are younger, you are less likely to go through menopause too soon because of chemotherapy.
People who go through chemotherapy and start having periods again may go through menopause many years earlier than others. To avoid losing the ability to have children because of chemotherapy.
Before starting chemotherapy, some people take pills that stop their periods for a short time; This is done to keep the ovaries and, in turn, the eggs from getting hurt. Before beginning cancer treatment, some people also choose to have their eggs frozen.
How Long Does Chemo-Induced Menopause Last?
Chemotherapy drugs often cause women to go through the symptoms of menopause at a much younger age. We call this effect of chemotherapy on women “chemo-induced menopause.”
When you think about chemopause, the menopause that happens after a woman undergoes chemotherapy, it can be hard to understand. It helps to be ready by knowing what to expect and why it will happen.
When a woman’s ovaries stop making the hormones estrogen and progesterone, this is called menopause. During this time, your ovaries also get smaller. Because of these changes, your menstrual cycle will become irregular and may even stop. A woman who hasn’t had her period for a year is said to be postmenopausal. In 2022, researchers found that 51 was the average age of menopause.
Cancer treatment can speed up the beginning of menopause. Studies in 2011 show that hot flashes and night sweats are among the vasomotor (VMS) symptoms of chemopause and menopause. The main cause of vasomotor symptoms is that blood vessels narrow and widen.
Menopause is a normal part of getting older, but the side effects that come from chemotherapy may seem worse. A study carried out in 2020 found that women who went through menopause because of chemotherapy had more hot flashes and felt more tired than women who went through menopause naturally.
When treating cancer, doctors often use drugs that are part of chemotherapy. The National Cancer Institute says that these medicines work because they eliminate cancer cells in the body. Chemotherapy is mostly about killing cells that divide quickly. So, it is also bad for the cells in your body that make hair. Chemotherapy could hurt your hormone levels and your reproductive organs, such as your ovaries.
Chemotherapy can mess up your hormone system while adding an imbalance of estrogen and progesterone. Chemotherapy can kill cells and mess up hormones, which can cause menopausal symptoms like irregular or stopped periods.
If you are over 40 when you start chemotherapy, your hormone levels may already be low. If your body has already started to go through menopause, chemotherapy may only speed up the process.
Symptoms Of Chemo-induced Menopause
Symptoms of chemopause are very similar to those of menopause. Your hormone levels may drop quickly instead of slowly, which makes the signs and symptoms seem worse. The common symptoms are:
-
Changes in menstrual cycles
-
Mood swings
-
Depression
-
Bipolar disorder.
-
Painful Sexual intercourse
-
Change in texture hair or loss of hair
-
Urinary system illnesses
-
Weight gain.
Chemotherapy can cause menopause in women, which can be temporary or last long. After you finish chemotherapy, it could take anywhere from a few months to two years for your periods to come back.
In 2015, scientists looked at 280 breast cancer cases in women younger than 45. There were 255 cases of chemo-induced menopause, in which the patient’s periods stopped for more than three months after treatment ended. But 170 people who took part said they had started menstruating again. Eighty-four percent of women who went through chemo-induced menopause never got their periods back.
The study shows that if you’ve had chemotherapy, your period might not come back as it did before. Today, most of what we know about periods after chemotherapy comes from anecdotes.
Ways To Reduce The Effects Of Chemo-induced Menopause
Management of menopause and chemopause are different in some important ways. Some hormone replacement drugs and mood stabilizers might not be a good idea during chemotherapy or when cancer is in remission.
A woman will often go through menopause because of chemotherapy. After treatment, it’s not a given that your period will come back, but it is possible. In addition to the side effects of the chemotherapy, some people may also have more intense menopause symptoms as their body system adjusts to a big hormone change; you can expect to see effects from chemotherapy, but your doctor and the rest of your cancer treatment team will help you prepare for them. You can treat menopause symptoms with natural therapies and medications, botch you should talk to your doctor about it.
- Dietary supplements
Dietary supplements can help make up for the fact that chemotherapy can mess with your hormones.
If you often suffer from night sweats and hot flashes, you could try taking a small amount of vitamin E to see if that helps. Osteoporosis is more common after menopause, but you can protect your bones with vitamin D and a calcium supplement.
Some anecdotal evidence suggests that black cohosh and dong quai help alleviate symptoms.
- Therapies that are used along with traditional medicine
Several types of complementary and alternative medicine may also help you feel better. Acupuncture is often used to help people with hot flashes and trouble sleeping. A 2014 study found that yoga can help women undergoing menopause live better lives.
- Alterations to your lifestyle
Modifying your lifestyle, such as avoiding alcohol and spicy foods, using a fan in your sleep, and decreasing the temperature in your house, will help alleviate hot flashes if they are mild to moderate.
Maintaining a healthy weight and regular aerobic and weight-bearing exercise can help you manage your mental and physical health.
- Hormone treatment
Hormone replacement therapy (HRT) is a way that some women deal with the symptoms of menopause. People with estrogen-sensitive cancer are often told not to take these drugs because they may make them return.
Hormones are used as part of medical treatment. Some women find that their hot flashes and other symptoms go away after their doctor puts them on a schedule of female hormones. But hormones come with some risks, and people who have had certain types of cancer may not be able to take them.
- Estrogen
Even if you can’t take hormone treatment, you can relieve dryness in the vagina by putting a very small amount of estrogen on the skin or injecting it into the vagina. These hormones can be put on the skin, taken by mouth, or put on a ring. You can only get these medicines if your doctor or other healthcare provider gives you a valid prescription.
- Antidepressants and other medicines.
If you can’t take hormones, your doctor may suggest an alternative treatment, like an antidepressant, for your hot flashes (even if you are not depressed). Even if you are not sad, these chemically-caused benefits of hot flashes may help you.
- Lotions or lubricants that keep skin moist.
If the mucous membranes in your vaginal area are dry, these products can help. Find a water-based lubricant like K-Y Jelly or Astroglide. Use something like Replens to moisturize your vaginal area once every few days instead.
Healthy Ways To Manage Menopause Symptoms
- Regular physical activities.
Regular exercise can help the process go more smoothly by making you less anxious and happier. Regular exercise can also help stop the weight gain and muscle loss that are common side effects of menopause.
The Centers for Disease Control and Prevention (CDC) recommend that healthy women do at least 75 minutes of vigorous exercise or 150 minutes of mild exercise.
Types Of Exercises

- Breathing exercises
Instead of breathing into your chest, focus on making your stomach and lower ribs bigger as you breathe in. Try lying on your back with your legs bent and putting one hand on your chest and the other on your belly; This is a simple way to start becoming aware of your breathing.
You’ll be able to do this kind of deep breathing in any position after you’ve done it a few times. This kind of conscious breathing can help relieve stress and may even make hot flashes less painful. You can’t stop a hot flash by breathing, but you can learn to deal with them better by breathing through them instead of fighting them.
You can start by lying on your back with your knees bent, one hand on your chest, and also on your stomach; This will help you understand the different ways your body can breathe. This method of careful breathing can help relieve stress and even make hot flashes less painful. Breathing won’t stop you from having a hot flash, but it can help you deal with them better, so you don’t make things worse by trying to fight them off.
- Cardio aerobic exercise
Cardio Aerobic exercises race up your heart rate and work your bigger muscles. Any activity that raises your heart rate will do the trick. Most of the time, any action can count.
- Walking
Your mental health, physical health, and blood pressure may all improve if you go for a walk. The best thing about going for a walk is that you can spend quality time with your friends, many of whom may be going through the same things you are during menopause. Adding a social element to your walk makes you likely to stick to your walking routine.
- Strength Training
The Centers for Disease Control and Prevention (CDC) recommends that people who have never exercised before start with not less than 10 minutes of light activity and gradually increase the intensity as it gets easier.
Strength training is especially important after menopause because women are more likely to get osteoporosis (estrogen is required to help lay down bone). With regular strength training, you may be able to get stronger bones and muscles, burn more fat, and speed up your metabolism.
At home, you can work out with dumbbells and resistance tubing. You can use either weight machines or free weights to build muscle at the gym. Choose a weight that will make your muscles work hard after 12 reps, and then go from there.
- Yoga
Since no two menopause transitions are the same, the ways you treat your symptoms should be based on your situation. If deep breathing, yoga, or meditation don’t work, try something else.
Restorative and supported yoga poses might be able to help. If you practice these positions, you might find peace and stability in your mind. They can also lessen the severity of symptoms such as:
-
High body temperature
-
Irritation
-
Tiredness.
- High-impact workouts
Due to menopause, the chances of getting weak bones and breaking them are much higher. High-impact workouts, like soccer, tennis, aerobic dancing, or hiking, are the best way to keep bone mass because they strengthen bones while working against gravity. Repeated impact, like what you get when you change direction, move from side to side, or make sudden changes, is good for bone health.
- Pelvic floor exercise
During perimenopause and menopause, hormonal changes can worsen urinary dysfunction and pelvic organ prolapse. They can also disrupt or cut off blood flow to the pelvic floor and weaken the vaginal mucosal tissues. Kegels and other exercises that work the muscles that hold up the genitalia can help with mobility, strength, coordination, and blood flow. Studies show that postmenopausal women who do pelvic floor exercises regularly feel more sexual pleasure and excitement.
- Dancing
Dancing doesn’t have to be hard if you work out with it. Adding a cardio workout to your daily routine could be a great way to burn calories and have fun simultaneously. If you don’t enjoy running on a treadmill, you could try taking a dance class. Dance is also a good way to build strength and improve flexibility. Find a style that suits you: jazz, ballet, or salsa.
- Elliptical trainer and StairMaster.
Remember that elliptical or StairMaster workouts are still good for you. You don’t have to pound the pavement to get a cardio workout. You can do it at the gym.
The risk of (CVD) cardiovascular disease increases significantly during menopause, according to the American Heart Association (AHA). During menopause, thermogenic levels are linked to better heart health. To keep your heart healthy, you need to be aware of possible risks and live a heart-healthy lifestyle.
- Resistance Exercises
Lifting heavy weights is the most effective exercise you can do. Weight training not only helps build muscle but also strengthens the bones and prevents future problems with the muscles and bones. You should switch things up if you’ve been doing the same workout with the same weights for a while. The idea is to train for less time with heavier weights.
If you usually use a 5-pound weight, you should do 12 sets of bicep curls or shoulder presses with an 8-pound weight. If you want your body to change in a good way, you need to push yourself until you think, “I can’t act like another rep.” It would be best if you moved to a heavier weight when your previous weight seems easy to lift, usually after two months of training.
- Zumba
Over the past 10 years, about 12 million people have stuck with the Zumba dancing fitness program. Zumba is a dance-based fitness program that people of all ages can do. You can work out your muscles and lose weight by moving to upbeat Latin music.
- Housework or yard work
Even if you only dust a little bit here and there, it doesn’t rent. However, what counts is if you work hard around the house or yard. Housework or hard yard work, like quads, core, and glutes; This kind of exercise, will help you. Start with 10 minutes of easy movement, add more time to your workouts and make them harder as it gets easier.
- Reducing Stress
Due to the changes in hormones. Some people’s symptoms can worsen, whether from menopause or something else; This is why it’s so important to find ways to relax right now; This will not only help with the symptoms of menopause, but it will also make you happier and better able to deal with the stresses of everyday life. Below are ways to deal with the stress and worry you might feel during menopause.
There are many ways to deal with stress;
- Yoga
Yoga is a kind of movement that isn’t too hard and may help you feel calm at this time. It’s also a good way to start a workout. Some people like the slower pace of Hatha Yoga, which focuses on calming both the body and the mind. This type of mental and physical balance training can significantly affect how much stress you feel. Regular exercise benefits go beyond the immediate health benefits.
- Exercise
Most women going through menopause don’t put a lot of thought into working out hard. But try to get some exercise every day; This will help you feel better by making your body make endorphins. Some people feel better emotionally and physically when they do this. The body’s sleep cycle is also helped by regular exercise.
- Meditation
The mind is equally as important as other parts of the body. Some people find that regular meditation helps them reach a deep level of relaxation, which in turn helps them deal with stress and feel more at ease in their daily lives.
- Massage
A good massage does two things: it relaxes your muscles and helps your body get rid of toxins that have built up. Your body will thank you for the time you spend here. It will feel calm and refreshed; a massage works so well to relieve stress, anxiety, and high blood pressure.
- Getting enough sleep.

You can try the following things besides taking medicine to help you sleep better and stay cooler at night:
-
Keep the temperature and air airflow in your bedroom just right.
-
Avoid spicy foods and other things that might make you sweat more right before bed.
-
To sleep well, it’s best to wear clothes that don’t fit too tightly. Most of the time, it’s best to wear clothes made from natural fibers like cotton.
-
Endeavor to go to bed every night at a fixed time.
-
It’s not a good idea to do anything before bed, like eating, reading, or watching TV. Do these things in a separate room to make yourself sleepy.
-
You might not sleep well at night if you take naps during the day, so try to avoid them if you can.
-
Keep a regular exercise schedule, but don’t do it right before bed.
-
It is suggested that you talk to your doctor about sleeping aids.
-
Always make sure your bladder is emptied before you go to bed.
- Quit smoking
Women who smoke have worse hot flashes, night sweats, and trouble sleeping. They also have them more often and more intensely.
The use of tobacco is bad for health all over the world because it hurts so many different parts of the body. Cigarette smoking is linked to acute myeloid leukemia and cancers of the lungs, larynx, mouth, throat, kidney, bladder, liver, pancreas, stomach, cervix, colon, and rectum.
Smoking exacerbates asthma in adults and causes or worsens COPD (chronic bronchitis and emphysema), diabetes, osteoporosis, rheumatoid arthritis, age-related macular degeneration, and cataracts. People who smoke are more prone to pneumonia, tuberculosis, and other lung diseases. Also, smoking causes inflammation and makes the immune system less strong.
Researchers once found that smoking cigarettes made it more likely that someone would get osteoporosis. Several studies have shown that smoking makes bones less dense. It’s hard to tell how smoking affects bones.
The size of their waists is another difference between people who smoke and people who don’t smoke. Even if they don’t smoke much, they are still more likely to get type 2 diabetes. If you already have diabetes, smoking will make it much harder to control the disease. Diabetes can lead to blindness, heart disease, kidney failure, and amputations.
- Avoiding hot flash triggers like coffee, tea, and alcohol.
People have used tofu and soybeans as an alternative treatment for vasomotor symptoms like hot flashes and to help them sleep. Phytoestrogen is a plant hormone that is found in soy products. It works more mildly, like estrogen.
A study showed that eating foods can cause hot flashes, night sweats, and mood swings. It’s possible that if you eat late at night, you’re more likely to get hot flashes.
Effects Of Lifestyle Practices On Menopausal Symptoms
Here are a few practices that trigger menopause symptoms and their effects:
| 1. | Coffee | Caffeine and alcohol, as well as sugary and spicy foods, are major hot flashes triggers. Women who go through menopause and regularly drink coffee, tea, or soda have worse hot flashes and night sweats than those who don’t drink caffeinated drinks. |
| 2. | Tea | Some teas and medicines don’t mix well with each other. If you want to take tea, you can talk to your doctor about how much tea you drink because some teas can thin the blood. Hot teas should be avoided, especially if your main symptom is hot flashes, because your flashes and night sweats may happen more often; This is true if you drink it right before bed. |
| 3. | Alcohol | Scientists have found that drinking alcohol might make it harder to get a good night’s sleep. Some people also think thanking red wine is a major cause of hot flashes. Women who regularly drank alcohol were likelier to have hot flashes and night sweats. |
| 4. | Smoking | By smoking, the hormone estrogen in women is lowered. Low estrogen levels can cause dry skin, hair loss, and trouble remembering things. One of the many bad things smoking causes to your health is heart disease. |
Conclusion
Menopause caused by cancer can be very painful, but estrogen and progesterone hormone replacement therapy can greatly reduce the symptoms. Because HRT is complicated, it is best to talk about it with a medical doctor one-on-one. Hormone replacement therapy (HRT) is an option for people with cancer.
Some women get relief from non-hormonal treatments, like antidepressants. One study found that the number of hot flashes in women who took antidepressants every day went down by 61%. Antidepressants may also help with the ups and downs of mood that are common during menopause.
Some women also choose indirect ways to deal with menopause. These could be by avoiding spicy foods, caffeine, and alcohol.







