Welcome to The Anti-Aging Center at Make You Well Advanced Anti-Aging, Hormone Therapy, and Medical Weight Loss in Torrance, CA Read more...
I’m a Woman Seeking Answers
You’re not crazy. You’re not alone.
You’re in the right place.
Menopause can feel confusing and lonely. We’re here to help you feel understood, supported, and connected to a real community that cares.
I’m a Healthcare Provider
Empower your practice with
menopause expertise.
Support your patients with confidence. Access expert tools, trusted training, and join a professional network focused on better menopause care.
Menopause - The Latest News and Resources
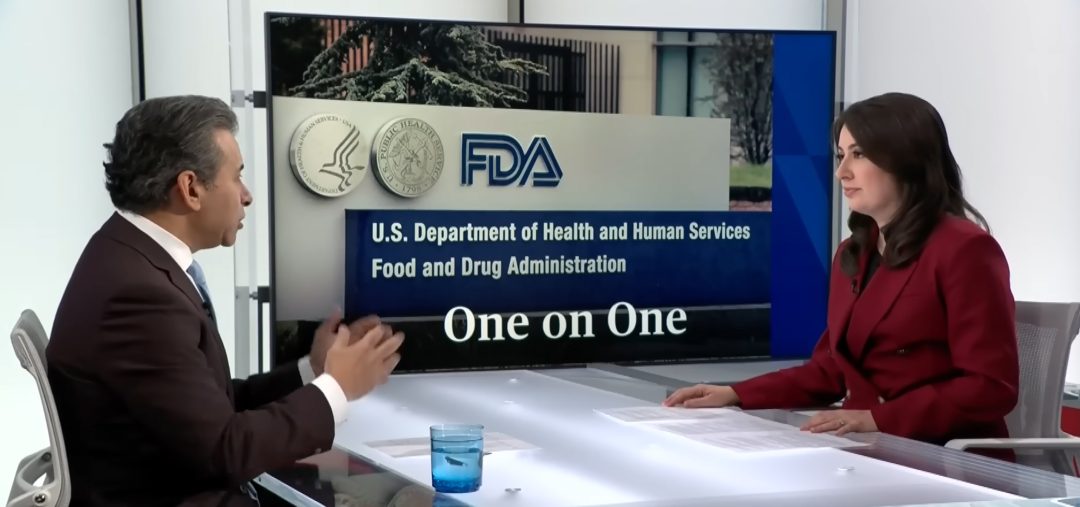
RFK Jr. and FDA Officials Make Announcement on Women's Health
Expert Panel on Menopause and Hormone Replacement Therapy for Women
A high-profile FDA panel convened in July 2025 sparked a pivotal public reckoning with the way hormone replacement therapy (HRT) for menopause is regulated and understood in the U.S. Leading experts challenged outdated warnings rooted in decades-old studies, highlighting mounting evidence for the safety and benefits of modern HRT—especially when initiated early. The meeting underscored both the scientific and human costs of regulatory inertia, signaling a major shift in national menopause care.
Correcting the Record: Re-evaluating the Risks and Benefits of Menopausal HRT
Dr. Hirsch challenged the outdated fear surrounding hormone therapy, especially the legacy of the WHI study. She called for removing the black box warning and advocated for patient-centered care, emphasizing the importance of educating both clinicians and the public with current evidence.
Read more
Beyond the WHI: Modernizing FDA Warnings on Hormone Therapy
Dr. Levy addressed the FDA’s black box warning, arguing it fails to reflect modern science. She focused on the distinction between systemic and local hormones and urged the FDA to revise its labeling to prevent unnecessary suffering and restore trust in HRT.
Read more
Women’s Access and Policy Reform: Why Black Box Warnings Must Change
Dr. Pinkerton delivered a powerful call to action, urging removal of the black box warning on hormone therapies. She emphasized the proven benefits of early intervention and called the outdated label a barrier to equitable, evidence-based care for millions of women.
Read more
Timing Matters: When and How HRT Delivers the Greatest Benefit
Dr. Simon highlighted how the timing of hormone therapy dramatically affects risk and benefit. With proper initiation and patient selection, he argued, HRT is both safe and effective—and current policy should reflect this individualized, modern approach to care.
Read more
More Than Symptoms: HRT and Mental Health in Menopause
Dr. Sarrel reframed menopause as a public-health crisis when left untreated. He emphasized HRT’s role not just in symptom relief, but in improving mood and reducing anxiety, calling for broader recognition of its mental health benefits in regulatory policy.
Read more
New Frontiers: Menopause, HRT, and the Female Brain
Dr. Brinton presented compelling research linking menopause-related hormone loss to Alzheimer’s risk. She explained how timely hormone therapy may protect brain function and called for smarter regulation that reflects newly emerging neurobiological evidence.
Read more
Bones at Risk: Estrogen, Osteoporosis, and Why Timing Counts
Dr. Wright focused on estrogen’s bone-preserving power, presenting HRT as the most effective therapy for preventing fractures. She argued that the black box warning deters life-saving interventions and must be removed to improve aging outcomes for women.
Read more
Testosterone Inequality: The Gender Gap in Hormone Care
Dr. Casperson highlighted gender disparities in hormone access, particularly the FDA’s failure to approve testosterone for women. She underscored how regulatory bias leaves women under-treated and pushed for fair, evidence-based therapeutic options.
Read more
Debunking Myths: Why the Black Box on Vaginal Estrogen Endangers Women
Dr. Minkin debunked myths about vaginal estrogen and condemned the black box warning as unsupported and damaging. She emphasized that low-dose vaginal therapy is safe and critical, and that outdated warnings harm both access and public perception.
Read more
Skepticism to Science: The Real Risks and Benefits of Local Estrogen Therapy
Dr. Rubin argued that vaginal estrogen is both essential and safe, yet remains stigmatized by outdated labeling. She showed the costs—clinical and economic—of withholding proven therapies, and advocated for removing regulatory barriers to access.
Read more
All-Cause Mortality and CVD: The Timing Hypothesis in HRT
Dr. Hodis emphasized that hormone therapy, when started early, improves survival and lowers cardiovascular risk. He advocated for a stratified approach to HRT labeling and urged the FDA to align regulatory guidance with decades of timing-specific data.
Read more
Menopause - News and Articles Sourced From Around the Globe
providers
Medical Spa
We offer luxurious spa services at unbeatable prices! Let our Licensed, experienced therapists help you relax, ease your stress, and Read more...
Phone: 8134756996
- Max Thakkar
Hormone Therapy
Meet Your Provider, Maranda S. Carlile FNP-BC Maranda is a board-certified family nurse practitioner. She graduated in 2016 with her Read more...
Phone: 435-565-1384
- Maranda Carlile
Women's Health
About Dr. Nicole Tully My name is Nicole Tully, MD and for almost 20 years, I have focused on Women’s Read more...
- Nicole Tully, MD
Hormone Therapy
You’ve got symptoms. We want to help. BodyLogicMD may help you get to the root causes of symptoms so you Read more...
Phone: (239) 206 - 4157 opt. 1
- Robert Rubin
Women's Health
We are a center supporting women from puberty to post-menopause. We offer pregnancy and lactation services, perimenopause and menopause support, Read more...
Phone: 2068194575
- Tracy Corey
Medical Spa
At J Sterling’s Spas you get affordable luxury. Treat yourself to 1Hr Massage or Facial starting from $45 and No Read more...
Phone: (407) 775-2620
- Max Thakkar
Cosmetic Surgery
Jim Brantner M.D. Plastic & Reconstructive Surgery in Johnson City, TN, helps patients look and feel their best. Jim Brantner Read more...
Phone: 4233289000
- Jim Brantner
Women's Health
About Midlife Midwife Functional Health At Midlife Midwife Functional Health, women in their 30s, 40s, and beyond finally find what Read more...
Phone: (571) 252 - 9779
- Donna Figueroa, CNM, FMACP, MSN, APRN
Functional Medicine
Meet Natasha My own “journey” began over two decades ago when I started my career in a compounding pharmacy. After Read more...
Phone: (877) 850-2580
- Natasha Mankins
Aesthetics
Dr. Christopher D. Marshall, M.D. Dr. Marshall received a Bachelor of Science in Biology and a Bachelor of Arts in Read more...
Phone: 731-257-1500
- Chris Marshall
Family Practitioner
Individualized Wellness Plan Hormone and Wellness Support Schedule a Consultation with an Experienced Board-Certified Licensed Family Nurse Practitioner Read more...
Phone: 207-249-6610
- Jennifer Gaulin, NP-C
Massage Irving, TX: Discover the Ultimate in Relaxation with Bluebonnet Searching for the perfect ‘massage near Irving, TX’ or a
You’ve got symptoms. We want to help. BodyLogicMD may help you get to the root causes of symptoms so you
Meet Dr. Craig Colville What is “the power of change?” It’s the philosophy that guides Dr. Craig Colville, one of
About Lakeside Holistic Health, PLLC Unlike conventional medicine that focuses more on the diagnosis and prescription, our team at Lakeside
About Dr. Nicole Tully My name is Nicole Tully, MD and for almost 20 years, I have focused on Women’s
At Hodari MD Dermatology & Rejuvené, board-certified dermatologist Dr. Kafele T. Hodari offers state of the art treatments, the finest
Dr. Tatiana Fleischman Founder and Medical Director Dr. Tatiana Fleischman is a medical doctor (MD) with special focus on Anti-Aging
At Emerald Waters Hormone & Weight Loss Clinic, our mission is to enhance the health, well-being, and overall quality of
The group of board-certified plastic surgeons at The Wall Center for Plastic Surgery has more than 50 years of combined
You’ve got symptoms. We want to help. BodyLogicMD may help you get to the root causes of symptoms so you
Discover a new approach to healthcare The Columbia Center for Integrative Medicine (CCIMHealth) is an integrative internal medicine service that
Pricilla Piñero, MSN, FNP-BC Founder of Infinite Quest Health & Wellness Pricilla Piñero is a bilingual Hispanic/Latina board-certified Nurse Practitioner
Videos Provided by Members
Slings and Mesh for Treating Incontinence
Dr. George K. Ibrahim
Biltmore Restorative Medicine
Hormone Replacement Therapy Benefits for Women
Dr. Julian R. Gershon Jr.
Aspen Institute for Antiaging and Regenerative Medicine
Empowering Women Through Hormone Replacement Therapy in 2025
Dr. Julian R. Gershon Jr.
Aspen Institute for Antiaging and Regenerative Medicine
You’re eating well, exercising, and doing everything “right.” So why are you still struggling with stubborn weight gain, mood swings,
Menopause marks more than hormonal change. It accelerates aging at the cellular level. Most women experience menopause as hot flashes,
Article Insights & Reflections Synopsis: This piece examines why conventional hormone therapy often falls short in addressing menopause symptoms comprehensively.
According to the Mayo Clinic, for women between the ages of 19-60, uterine fibroids may be a reality of life.
Article Insights & Reflections Synopsis: This overview brings clarity to a key menopause topic and translates research into practical next
Finally. When I heard the FDA removed those misleading warnings on hormone therapy, that was my first thought. Anyone who
Loading...